Research Article - Journal of Contemporary Medical Education (2023)
Utility of the Butterfly iQ Ultrasound for Resident and Medical Student Education
Nisha R Patel, Sheila Mullen, Bryanna McGowan, Aimee Thomas, Zuhaib Khokhar, Brett Ploussard and Emad Allam*Emad Allam, Department of Radiology and Medical Imaging, Loyola University Medical Center, Illinois, USA, Email: emad.allam@lumc.edu
Received: 08-Jul-2023, Manuscript No. JCMEDU-23-105327; Editor assigned: 13-Jul-2023, Pre QC No. JCMEDU-23-105327 (PQ); Reviewed: 27-Jul-2023, QC No. JCMEDU-23-105327; Revised: 03-Aug-2023, Manuscript No. JCMEDU-23-105327 (R); Published: 10-Aug-2023
Abstract
Objectives: Point-of-Care Ultrasound (POCUS) has been a rising development in the medical field. POCUS is considered to be an ultrasound brought to the patient and completed by the healthcare provider, as opposed to completed by a sonographer with the images sent to a radiologist for interpretation. Images are acquired and analyzed in real-time to help guide physicians in diagnostic and therapeutic management. In our study, we investigated the benefit of allowing radiology residents and medical students to train with the Butterfly iQ+ device at home to learn how the POCUS probe works, become familiar with its features, and practice scanning on their own.
Methods: Sixteen trainees participated in our study over the course of a year (14 residents, 2 medical students). Study participants were surveyed prior to and following self-directed use of the device.
Results: All participants reported that they would recommend the Butterfly iQ+ device to other residents and rated the device as 5/5 in terms of its use as a learning tool. A positive response to use of POCUS in training was observed in our study.
Conclusion: Our findings continue to support the growing need for a hands-on ultrasound curriculum. They also demonstrate the effectiveness of using a mobile ultrasound device for self-directed learning of ultrasound principles in healthcare training.
Keywords
Ultrasound; Healthcare; Training;Radiology; Learning.
Abbrevations
POCUS: Point-of-Care Ultrasound; IRB: Institutional review board; PGY: Post-graduate year.
Introduction
Point-of-Care Ultrasound (POCUS) has been a rising phenomenon over the past decade, and its use has increased dramatically over this time period. Point-of-Care Ultrasound (POCUS) machines have become smaller, more affordable, and easier to use, with some people referring to the devices as “the stethoscope of the 21st century” [1,2]. Point-of-Care Ultrasound (POCUS) machines have undergone advancements allowing them to scan at different frequencies, have multiple types of transducers, and take measurements. More recent developments have also included bi-plane scanning and spectral Doppler [1,2]. Due to these technological developments, ultrasounds can now be offered at medical sites that were previously unable to provide ultrasound exams [3].
Certain fields have widely adopted and implemented Point-of-Care Ultrasound (POCUS). Emergency department and critical care physicians are those who have seen the most effective use of Point-of-Care Ultrasound (POCUS) machines. These physicians have been able to show its usefulness as a diagnostic tool focusing on the chest, abdomen and proximal veins for DVT [2,4-9]. Point-of-Care Ultrasound (POCUS) has also been shown to be useful for procedural guidance, including peripheral and central vascular access, paracentesis, thoracentesis, regional anesthesia and lumbar punctures [2,6,7,9]. Point-of-Care Ultrasound (POCUS) has been found effective in the diagnosis of musculoskeletal injuries, with current literature documenting its usefulness in diagnosing ankle, knee, and shoulder injuries. The benefit of using Point-of-Care Ultrasound (POCUS) in these scenarios goes beyond its high diagnostic accuracy. It also decreases patient exposure to ionizing radiation and potentially reduces time to diagnosis and treatment in comparison to longer exams such as Magnetic resonance imaging (MRI) or Computed Tomography (CT) [10-15].
Large topics of discussion surrounding Point-of-Care Ultrasound (POCUS) include training resident and attending physicians to become competent in it and creating a standardized curriculum and credentialing system. Currently, there are no standardized guidelines for those who wish to use Point-of-Care Ultrasound (POCUS) in a clinical setting; thus, it is open for use by anyone. The American College of Radiology (ACR) however, does publish guidelines on the training and continued reading required to be proficient at interpreting ultrasound [16]. The Royal College of Physicians and Surgeons as well as the American College of Emergency Physicians have both created formal guidelines regarding the training and usage of Point-of-Care Ultrasound (POCUS) [16-18].
Our study aims to analyze the usefulness of self-directed learning in training in Point-of-Care Ultrasound (POCUS). We currently have the Butterfly iQ+ (Guilford, CT) device available in our radiology department. The device is one of the newer technologies in Point-of-Care Ultrasound (POCUS) and has many of the newer features available at this time. The machine also has a large bank of educational content available to the user. It provides videos for users of all levels, from instructions on how to use the device and adjust settings to videos demonstrating how to use the device to perform specific exams or examine certain body parts. We hope to find that through self-directed learning, residents and medical students are able to learn more about the capabilities of Point-of-Care Ultrasound (POCUS) and improve their ultrasound skills.
Methods
This study was Institutional Review Board (IRB) approved and was conducted by surveying participants via surveys created on Google Forms. Participants in this study included diagnostic radiology residents at Loyola University Medical Center and medical students at Stritch School of Medicine, Loyola University Chicago. Consent was obtained from all participants by the principal investigator. Participants completed a survey questionnaire prior to and after use of the Butterfly iQ+ device (Guilford, CT). Recruitment was conducted by the principal investigator in the radiology department. Interested participants were informed about the device and the study aims and requirements. Participants then enrolled in the study on a voluntary basis.
Once enrolled, participants filled out a pre-survey to obtain their name, gender, year of training, and consent for use of their feedback information for research purposes. A brief written guide and video tutorial were made available on the use of the Butterfly iQ+ device and application for mobile devices. Participants utilized the Butterfly iQ+ device at home and viewed instructional videos on their mobile device application at their own discretion. Upon returning the device, participants were given a post-survey to assess device usage. Length of device use, whom the device was used on (e.g. self, someone else, self and somebody else), number of instructional videos viewed on the mobile device application, and any technical issues were assessed. Participants were also asked to rate the device as a learning tool on a scale of 1 to 5 (1 being poor and 5 being excellent) and indicated whether or not they would recommend the device as a useful learning tool to other radiology residents. Data collected from this survey was used to analyze the usefulness of the device to residents and students.
Results
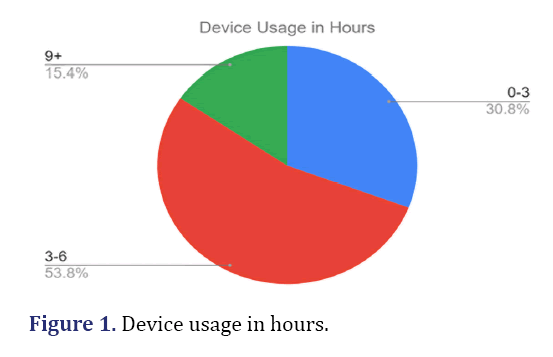
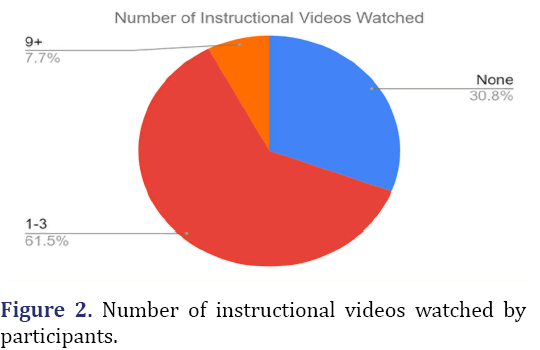
There were 16 responses including 14 residents and 2 medical students. Residents ranged from PGY-1 to PGY-5 while the medical students were in their fourth year. Three participants declined use of their feedback information for research purposes. The majority of residents used the Butterfly iQ device for 3-6 hours, and 50% of participants practiced using the device on themselves and on another person. The majority of participants watched 1-3 instructional videos on the Butterfly iQ app (Figures 1 and 2)
All participants rated the Butterfly iQ device as 5 out of 5 as a learning tool, and all participants indicated that they would recommend the device as a useful learning tool for other radiology residents. A PGY-3 resident remarked, “Love the idea of being able to trial the Butterfly US and practice scanning on my own time schedule. Great way to better conceptualize and understand the studies. The instructional videos are also a helpful asset.” A PGY-4 resident reported, “feeling much more confident with ultrasound”. Others expressed interest in using the device again and purchasing their own. A medical student commented on the user-friendly nature of the device, “Very compact device that has many features packed into one probe and is very compatible with a phone, making it easy to use.”
Conclusion
Despite the numerous recent developments of Point-of-Care Ultrasound (POCUS), there are still limitations to these devices, making traditional ultrasound more beneficial in certain situations. Point-of-Care Ultrasound (POCUS) machines still have lower image quality than traditional machines. Advanced imaging techniques such as transthoracic echocardiogram require the highest image quality available to provide cardiologists with the most information possible to aid in diagnosis and management. In one study looking at patients with inflammatory arthritis, a cart-based ultrasound machine was able to better detect power Doppler signal compared to the Butterfly iQ+ device. When comparing the Butterfly iQ+ device to a traditional ultrasound machine, no significant difference in patient evaluation time was noted.
Our study highlights the role of Point-of-Care Ultrasound (POCUS) in residency and medical student training. The emerging need for ultrasound calls for improved hands-on learning in this modality for learners in healthcare settings. Our study demonstrates the positive response residents and medical students alike had toward use of Point-of-Care Ultrasound (POCUS) in learning ultrasound.
Discussion
This study investigated resident and medical student responses to self-directed learning of Point-of-Care Ultrasound (POCUS) using the Butterfly iQ+ device. The Butterfly iQ+ device has been shown to be highly effective in various settings such as tele-guidance for remote military clinicians, emergency departments, imaging for vascular access, imaging of lungs in patients with COVID-19, and joint imaging in patients with inflammatory arthritis [3,10,19-21]. There have also been studies outlining Point-of-Care Ultrasound (POCUS) training for undergraduate and/or medical students and how training in ultrasound during this time can help them learn anatomy and improve their physical exam skills [5,17,22]. The effectiveness of handheld, portable ultrasound devices has been demonstrated even when compared to traditional ultrasound machines [20].
Education and usage of Point-of-Care Ultrasound (POCUS) has mostly been simplified to three main categories: image generation, image interpretation, and clinical integration. Because Point-of-Care Ultrasound (POCUS) is performed by the healthcare provider directly on a patient, providers must be skilled in all three phases of ultrasound in order to use Point-of-Care Ultrasound (POCUS) effectively. Many training programs have been outlined previously in the literature. These programs include the use of the machines with variable supervision or feedback vs. more self-directed learning with the machines. Others have proposed the use of ultrasound simulators to help emulate real-life scenarios [4,16,22]. Despite these proposed curriculums for Point-of-Care Ultrasound (POCUS) training and strong evidence supporting Point-of-Care Ultrasound (POCUS) use in various settings, no standardized protocol has been made to train or credential those interested in using Point-of-Care Ultrasound (POCUS).
Unfortunately, a barrier to more formal training in Point-of-Care Ultrasound (POCUS) is the lack of qualified instructors relative to the number of trainees and physicians interested in becoming proficient at Point-of-Care Ultrasound (POCUS). Some programs also suffer from lack of access to Point-of-Care Ultrasound (Point-of-Care Ultrasound (POCUS)) machines or limited educational time available for a formal training curriculum [22]. Currently, there are far more residents and residency programs that show an interest in formal Point-of-Care Ultrasound (POCUS) training than those that currently have a formal clinical curriculum for Point-of-Care Ultrasound (POCUS) training [23-27]. In our study, residents reported use of the device for multiple hours, and a large percentage of trainees voluntarily used instructional videos provided by the Butterfly iQ+ device mobile application. Residents and/or medical students particularly noted the device’s user-friendliness, its ability to allow for training/practice in a manner more congruent with their personal schedules, and its ability to improve their confidence in using ultrasound. Others also mentioned its use in helping with the conceptualization of studies, learning normal anatomy, and practicing ultrasound-guided procedures. Having received full endorsement by study participants in terms of ratings and recommendation to others, the Point-of-Care Ultrasound (POCUS) device appears to be highly regarded by trainees. Based on participant responses to our study, we believe self-directed learning can be highly beneficial for medical trainees in order to increase their familiarization with Point-of-Care Ultrasound (POCUS). A pilot study by the American Society of Echocardiography demonstrated notable differences in skill and knowledge test scores before and after students received online and in-person ultrasound training [28]. Due to the time and resource restraints associated with creating a formal curriculum, self-directed learning may be a reasonable alternative for residents and attending physicians interested in expanding their practice with Point-of-Care Ultrasound (POCUS).
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- Baribeau Y, Sharkey A, Chaudhary O, Krumm S, Fatima H, Mahmood F, et al. Handheld point-of-care ultrasound probes: the new generation of POCUS. J Cardiothorac Vasc Anesth 2020;34(11):3139-3145.
[Crossref] [Google Scholar] [PubMed]
- Moore CL, Copel JA. Point-of-care ultrasonography. N Engl J Med 2011;364(8):749-757.
[Crossref] [Google Scholar] [PubMed]
- Burleson SL, Swanson JF, Shufflebarger EF, Wallace DW, Heimann MA, Crosby JC, et al. Evaluation of a novel handheld point-of-care ultrasound device in an African emergency department. Ultrasound J 2020;12(1):1-5.
[Crossref] [Google Scholar] [PubMed]
- Johri AM, Durbin J, Newbigging J, Tanzola R, Chow R, De S, et al. Cardiac point-of-care ultrasound: state-of-the-art in medical school education. J Am Soc Echocardiogr 2018;31(7):749-760.
[Crossref] [Google Scholar] [PubMed]
- Cid X, Canty D, Royse A, Maier AB, Johnson D, El-Ansary D, et al. Impact of point-of-care ultrasound on the hospital length of stay for internal medicine inpatients with cardiopulmonary diagnosis at admission: study protocol of a randomized controlled trial—the IMFCU-1 (Internal Medicine Focused Clinical Ultrasound) study. Trials 2020;21(1):1-5.
[Crossref] [Google Scholar] [PubMed]
- Narasimhan M, Koenig SJ, Mayo PH. A whole-body approach to point of care ultrasound. Chest 2016;150(4):772-776.
[Crossref] [Google Scholar] [PubMed]
- Blanco P, Volpicelli G. Common pitfalls in point-of-care ultrasound: a practical guide for emergency and critical care physicians. Crit Ultrasound J 2016;8(1):1-2.
[Crossref] [Google Scholar] [PubMed]
- Lee L, DeCara JM. Point-of-Care Ultrasound. Curr Cardiol Rep 2020;22(11):1-10.
[Crossref] [Google Scholar] [PubMed]
- Zieleskiewicz L, Muller L, Lakhal K, Meresse Z, Arbelot C, Bertrand PM, et al. Point-of-Care Ultrasound in intensive care units: assessment of 1073 procedures in a multicentric, prospective, observational study. Intensive Care Med. 2015;41(9):1638-1647.
[Crossref] [Google Scholar] [PubMed]
- Corte G, Bayat S, Tascilar K, Valor-Mendez L, Schuster L, Knitza J, et al. Performance of a handheld ultrasound device to assess articular and periarticular pathologies in patients with inflammatory arthritis. Diagnostics (Basel) 2021;11(7):1139.
[Crossref] [Google Scholar] [PubMed]
- Hedelin H, Goksör LÅ, Karlsson J, Stjernström S. Ultrasound-assisted triage of ankle trauma can decrease the need for radiographic imaging. Am J Emerg Med 2013;31(12):1686-1689.
[Crossref] [Google Scholar] [PubMed]
- Secko MA, Reardon L, Gottlieb M, Morley EJ, Lohse MR, Thode Jr HC, et al. Musculoskeletal ultrasonography to diagnose dislocated shoulders: a prospective cohort. Ann Emerg Med 2020;76(2):119-128.
[Crossref] [Google Scholar] [PubMed]
- Situ-LaCasse E, Grieger RW, Crabbe S, Waterbrook AL, Friedman L, Adhikari S. Utility of point-of-care musculoskeletal ultrasound in the evaluation of emergency department musculoskeletal pathology. World J Emerg Med 2018;9(4):262-266.
[Crossref] [Google Scholar] [PubMed]
- Gottlieb M, Holladay D, Peksa GD. Point-of-Care Ultrasound for the diagnosis of shoulder dislocation: a systematic review and meta-analysis. Am J Emerg Med 2019;37(4):757-761.
[Crossref] [Google Scholar] [PubMed]
- Ghosh N, Kruse D, Subeh M, Lahham S, Fox JC. Comparing point-of-care-ultrasound (POCUS) to MRI for the diagnosis of medial compartment knee injuries. J Med Ultrasound 2017;25(3):167-172.
[Crossref] [Google Scholar] [PubMed]
- ACR–SPR–SRU practice parameter for performing and interpreting diagnostic ultrasound examinations. ACR
- Mackay FD, Zhou F, Lewis D, Fraser J, Atkinson PR, Atkinson P. Can you teach yourself point-of-care ultrasound to a level of clinical competency? Evaluation of a self-directed simulation-based training program. Cureus 2018;10(9):e3320.
[Crossref] [Google Scholar] [PubMed]
- Ultrasound guidelines: emergency, point-of-care and clinical ultrasound guidelines in medicine. Ann Emerg Med 2017;69(5):e27-e54. [Crossref]
[Google Scholar] [PubMed]
- Blenkinsop G, Heller RA, Carter NJ, Burkett A, Ballard M, Tai N. Remote ultrasound diagnostics disrupting traditional military frontline healthcare delivery. BMJ Mil Health. 2021.
[Crossref] [Google Scholar] [PubMed]
- Convissar D, Bittner EA, Chang MG. Biplane imaging using portable ultrasound devices for vascular access. Cureus 2021;13(1):e12561.
[Crossref] [Google Scholar] [PubMed]
- Bennett D, de Vita E, Mezzasalma F, Lanzarone N, Cameli P, Bianchi F, et al. Portable pocket-sized ultrasound scanner for the evaluation of lung involvement in coronavirus disease 2019 patients. Ultrasound Med Biol 2021;47(1):19-24.
[Crossref] [Google Scholar] [PubMed]
- Walker B, Barnes O, Deal O. Using point-of-care ultrasonography (POCUS) to empower medical education. Med Teach 2020;43(7):859.
[Crossref] [Google Scholar] [PubMed]
- Blans MJ, Pijl ME, van de Water JM, Poppe HJ, Bosch FH. The implementation of POCUS and POCUS training for residents: the Rijnstate approach. Neth J Med 2020;78(3):116-124.
[Google Scholar] [PubMed]
- Rajamani A, Miu M, Huang S, Elbourne-Binns H, Pracher F, Gunawan S, et al. Impact of critical care point-of-care ultrasound short-courses on trainee competence. Crit Care Med 2019;47(9):e782-e784.
[Crossref] [Google Scholar] [PubMed]
- Olgers TJ, Azizi N, Blans M, Bosch F, Gans RO, Ter Maaten JC. Point-of-Care Ultrasound (PoCUS) for the internist in acute medicine: a uniform curriculum. Neth J Med 2019;77(5):168-176.
[Google Scholar] [PubMed]
- Ambasta A, Balan M, Mayette M, Goffi A, Mulvagh S, Buchanan B, et al. Education indicators for internal medicine point-of-care ultrasound: a consensus report from the Canadian Internal Medicine Ultrasound (CIMUS) Group. J Gen Intern Med 2019;34:2123-2129.
[Crossref] [Google Scholar] [PubMed]
- Good R, Orsborn J, Stidham T. Point-of-Care Ultrasound education for pediatric residents in the pediatric intensive care unit. MedEdPORTAL 2018;14:10683.
[Crossref] [Google Scholar] [PubMed]
- Jujo S, Sakka BI, Lee-Jayaram JJ, Kataoka A, Izumo M, Kusunose K, et al. Medical student medium-term skill retention following cardiac point-of-care ultrasound training based on the American Society of Echocardiography curriculum framework. Cardiovasc Ultrasound 2022;20(1):1-2.
[Crossref] [Google Scholar] [PubMed]