Review Article - Journal of Contemporary Medical Education (2024)
Historical Perspectives in the Pedagogy of Anatomy Instruction in Medical and Graduate Education: From Salerno to Montserrat
Orien L Tulp*, George P Einstein, Frantz Sainvil, Hailin Wu and Rolando BranlyOrien L Tulp, Department of Medicine, University of Science Arts and Technology, Montserrat, USA, Email: o.tulp@usat.edu
Received: 03-Jan-2024, Manuscript No. JCMEDU-24-124351 ; Editor assigned: 08-Jan-2024, Pre QC No. JCMEDU-24-124351 (PQ); Reviewed: 22-Jan-2024, QC No. JCMEDU-24-124351 ; Revised: 29-Jan-2024, Manuscript No. JCMEDU-24-124351 (R); Published: 05-Jan-2024
Abstract
Because the including of human anatomy forms a core foundation for clinical medicine, it has contributed a pivotal role in medical education for many centuries. Thus, with advancements in the science of modern, current day medicine, its continued place in the medical school curriculum deserves careful attention. The recent pandemic has imposed additional stress and limitations on gross anatomy and other course modules. A seemingly ever-increasing emphasis on additional modules in molecular biology, emerging pharmacotherapeutics and pathophysiology content have resulted in a condensation and apparent erosion of previously allotted classroom and laboratory hours in the gross anatomy curriculum. To this end, technologic advancements including applications of virtual anatomy lecture and dissection elements, combined with small group dissections which emphasized relevant surgical and clinical applications with a surgical focus, pathophysiologic focal points, vascular and neural visualization techniques performed in fresh, non-embalmed cadavers. In addition, an imposition of financial constraints and a decreasing availability of sufficient cadaver donations to support gross anatomy dissection labs has also occurred in some locations. An innovative clinically focused cadaveric anatomy program is described which has improved the delivery and content retention of medical and graduate students and has become one of the most popular modules in the revised clinically oriented curriculum and has been deemed highly relevant to current medical education and graduate studies. The modifications to the anatomy curriculum have not only retained essential anatomic content but improved the overall interest in the importance of anatomy as an essential component of medical education, while improving the efficiency of delivery. The result was to enhance the overall level and effectiveness of instruction, while including a renewed focus on the clinical relevance of each system examined. As a result, the anatomy module transitioned to become one of the most sought-after components of the medical basic sciences portion of the medical curriculum.Keywords
Anatomy; Cadaveric dissection; Prosection; Virtual dissection; Clinical integration; COVID-19 pandemic; Fiberoptic examination; Surface anatomy
Introduction
Historically, the practice of anatomic cadaveric dissection has long been considered an essential component and necessary milestone in the medical education of aspiring physicians and biomedical scientists since the earliest recorded history of medical education. In ancient Egypt, cadaveric dissection originated as a religious ritual that was required as a rite of passage to the kingdom of the dead, where the procedure resembled more of a crude autopsy than an anatomical dissection as we might perform the process today. The earliest recorded medical school was founded in Salerno, Italy in 1235. In that program, cadaveric anatomy soon ascended to a prominent position in their medical curriculum. At Salerno, human dissection was performed as a sacramental procedure that illustrated the dissertations of revered ancient authors of the era. During the Renaissance, with the opening of the Anatomical Theatres in Padua (1490) and Bologna (1637), anatomy was considered an essential albeit artistic and spiritual exploration of the life, suffering, and death of the deceased, although most causes of death were then unknown. Anatomists began to dissect more extensively to investigate the structure of the body and produced texts that illustrated the images that were based on their dissections, and where such that pathological variations might be noted. The modern era of scientific aspects of human anatomy was highlighted by the publication of the main opera Anatomical Theatres in Padua who is considered prominent among the real fathers and ancestors of the scientific nature of modern anatomy as we know it today.
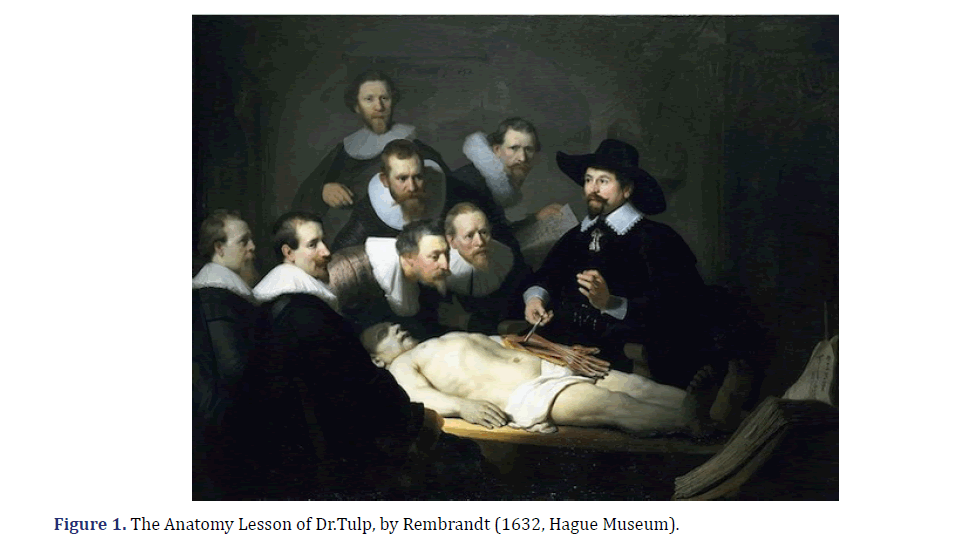
In the 17th century, the renowned Dr. Nicolaes Tulp, as a young, fledgling artist in his early 20s, painted his now famous rendition of cadaveric dissection. Renditions of his painting now adorn most modern anatomy departments. He was well known in Amsterdam as a practicing physician and surgeon. He was also a prominent civic leader and an anatomist who was appointed as praelector in anatomy. Among his duties and responsibilities were to regularize public dissections; he was also charged by the Surgeons’ Guild to apprentice new surgeons. Nicolaes Tulp (9 October 1593-12 September 1674) was a Dutch surgeon and the mayor of Amsterdam. Dr.Tulp was well known for his upstanding moral character and as the subject of Rembrandt’s famous painting The Anatomy Lesson of Dr. Nicolaes Tulp [1-4]. Dr. Nicholaes Tulp has since earned centuries of acclaim in medical anatomy following his famous rendition of a cadaveric dissection since first portrayed in 1832 while he was still the emerging artist we now recognize as Rembrandt. Thankfully the teaching of anatomy has enjoyed many advances in pedagogy and process since that time, although the basics displayed by Dr.Tulp remain important in today’s discussion [1,4]. The 18th to the 20th century saw a large expansion of medical schools throughout most countries of the world, each with their own model of inclusion of cadaveric dissection. Indications of religious overtones were sometimes noted, as cadaveric skeletal remains have recently been unearthed in Cambridge MA Holden Chapel and others, then the sites of early US medical schools [5-7]. Dissection instrumentation and decorum was similar to the surgeons’ tools of the day and has undergone vast improvements to the present day where it may resemble a modern surgical theatre with an expanded capacity of multiple cadavers simultaneously to accommodate the larger numbers of medical students now common to most Instructions. Moreover, since the outset of the recent COVID-19 pandemic, the incorporation of alternative strategies in the modernization and reorganization of anatomy curricula have placed increasing economic and didactic pressures on previously existing curricular models but have not outpaced the need for some back to the basic’s skills in dissection. Regional dissection is still what most surgeons and anatomists do best and may require more than just textbook and virtual illustrations for the developing practitioner or budding surgeon to excel in their career. In the recent past decades, the delivery of the gross anatomy course in medical and graduate education used to consist of 10 or more semester credit hours distributed over a full academic year of the curriculum.
However, the entire core course is now often reduced to a single semester. Recently, in an attempt to provide guidance to decision-makers involved in clinical anatomy curriculum development at the medical school level, the Educational Affairs Committee of the American Association of Clinical Anatomists (AACA) developed a document which defines the general contours of a gross anatomy curriculum designed to lead to a medical degree. The main body of the document establishes the anatomical concepts as well as the subject matter a student should master prior to graduation from medical school. Gross anatomy dissection is still a crucial primary core topic in medical school and biomedical graduate studies. The nature and content of gross anatomy, which was historically regarded as a core course in biomedical education in MBBS, MD, DO, and some PhD and Graduate curricula as well as in other disciplines of selective graduate education and non-allopathic medical programs, were significantly impacted by emerging challenges in the pedagogy of delivering medical education during the recent pandemic, which impacted many areas of medical and graduate education. Restrictions were imposed on group size and social distancing, which enabled innovative reexamination and restructuring in the delivery of instructional modules in aspects of both didactic and gross dissection activities. Moreover, the travel and public assembly restrictions forced by the pandemic required the adoption of off-campus modules for much of the traditional lecture content and limited the opportunities for the dissection element of the instruction. This mandated adjustment has included substantial reduction in both didactic lecture availability and laboratory dissections that were once a major core course and the major hallmark of a first-year medical student’s and some graduate student’s academic pursuits [8-14]. The results are that the role of gross anatomy as a core course in the medical curriculum has been forced to undergo much needed and welcome transition in scope and content in many institutions around the globe based on a variety of economic, epidemiological, and other factors [14].
With great advancements in educational technology and in the overall content and complexity and a drive toward a more clinically oriented focus of basic medical sciences in recent decades, the necessity for broad progressive updates and topic integration has now assumed an urgency in curriculum development. Because a fewer number of the generous clock hours previously allocated for gross anatomy instruction still remain available, the necessity for close review of the most essential topics, critical course content and compressed time for laboratory sessions are now imminent. It is noteworthy that the overall subject content, depth of instruction and student comprehension in the developing current curricular models has not diminished, while student expectations have likely increased. If anything, the overall content has not only maintained its overwhelming criticality in importance, but it has also increased in its complexity in its potential applications [15]. Therefore, a driving need exists to condense such courses into shorter time frames and clock hours of participation to the extent possible. These benefits may be attained by making more efficient use of resources to include the incorporation of a stronger clinical focus, by integrating computer-assisted virtual applications, simulation exercises, 3-D modeling, Problem-Based Learning (PBL) approaches, and by adding a presurgical approach to the laboratory modules by including surgical theatre demeanor and clinically relevant procedures [15,16]. The net result of the above is geared toward providing a stronger and more appropriate instructional program that is more closely related to the current time, period, and circumstances of contemporary interest. By offering more relevant content and technologically enhanced quality of medical education an institution may better meet the challenges and success on qualifying examinations the future may present to the new medical or bioscience graduate [17].
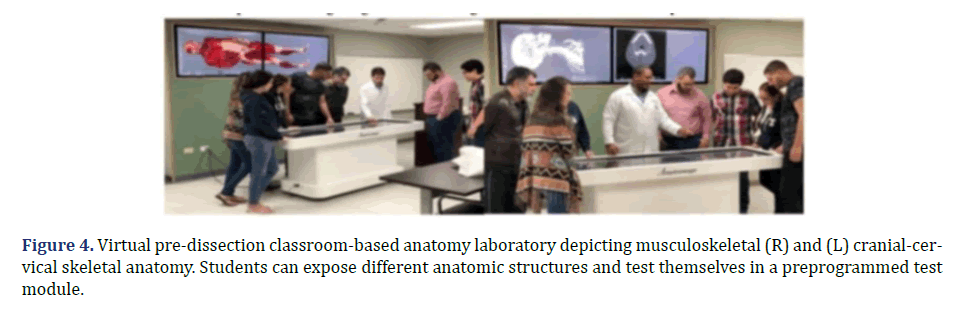
If the above objectives are achieved, including presenting the resulting course content in the most imaginative and cost- effective manner possible within the available time constraints, students should be able to complete their primary medical or graduate qualification and subsequent graduation from medical or graduate school within the current 4 or more years, depending on the nature of the program (i.e., MBBS, MD, PhD, or combined program). To accomplish these objectives, the didactic lectures are often integrated and oriented along organ system-based settings for each phase of the lectures. Lectures are followed by a virtual anatomy system such as Anatomage® or similar virtual instructional assist and organized with a clinically oriented Problem-Based Learning (PBL approach) with a defined clinical focus and clear objectives and end points in mind [18-20]. Discussions are best conducted in small groups, where the student to instructor ratio remains under 8:1. And encourages optimal student faculty interactions when discussing critical points. The presentations welcome topics in Pathophysiology, Medical Biophysics, Medical Epidemiology, and preclinical introduction to selected clinical procedures. The discussions may be integrated where appropriate to further broaden the scope of the lesson to include other areas of allopathic and natural medicine [20]. Upon completion of the dissection exercises, each student is expected to be able to demonstrate the above procedures to a defined standard, including a complete functional surgical dissection, in addition to other ancillary techniques such as suturing and forensic observations, often best accomplished with non-embalmed cadavers, which can add additional realism and clinical focus to the process [18-21]. The anatomic content is reinforced and revisited in subsequent years in basic science and clinical modules [18]. With careful attention to planning, and adherence to the curriculum one can likely fulfill the needs of tomorrow’s medical practitioners, surgeons, physicians, and biomedical scientists; with careful attention to content and need. To accomplish the academic challenges successfully will require the undeterred will and motivation of a dedicated faculty and staff, and availability of emerging educational technologies now available. With such resources in mind, one can help to attain and maintain the challenge that will enable the students of today and tomorrow to master the field of anatomy, physiology, neurobiology and associated topics [22,23].
The recent emergence of the recent coronavirus pandemic and other endemics have now added an additional extraordinary burden to compressing the educational process by forcing compromises in classroom and laboratory participation. Reliable cadaver availability and cadaver safety issues have also been impacted by the above factors, and collectively have further impacted negatively on cadaver availability [14,21]. The greater challenge however may be progressive schedule reallocations of laboratory hours with decreases for some subjects that previously could be allotted to the cadaveric dissection experience timeslot [9,10,16]. Since retiring faculty may not always be replaced with the same disciplines, talents, experience levels and specializations as in the past, adequate supervision of cadaveric anatomy may also become compromised, as cadaveric labs require adequate supervision and safety concerns, thereby placing further constraints on opportunities for individualized modes of instruction where unique dissecting skills and surgical techniques may be gained [13,14]. In contrast, a computer-based laboratory may bypass many of the safety and availability concerns noted above. Moreover, by incorporation of the computer based virtual addition, the scope and cost effectiveness of the laboratory may be further improved by combining students of other relevant career fields and their interests in instruction.
There are several key objectives one might consider in the design, conduct, and projected outcomes of anatomy instruction in the 21st century as discussed in detail elsewhere, including [18-20]:
1. Determine and clarify the learning objectives at the outset of the course; include safety concerns as an essential element at all levels of the process. Anatomy laboratory is one of the most high-yield experiences students may encounter in their formative years of basic medical sciences.
2. Determine the duration of the projected pre-dissection and dissection experiences, the goals one wishes to accomplish, and what the desired critical endpoint should be?
3. Include a Clinically Oriented Focus when planning and conducting the dissection laboratory.
4. Identify the budget availability and limitations, as the laboratory experiences tend to be more expensive than typical wet labs. Budgetary constraints must be considered in advance.
5. Plan the structure of the pre-dissection and dissection components such that they may continue to be relevant in later modules; identify risks, benefits, and restrictions if any.
6. Cadaveric dissection is an intense, focused experience regardless of group size, and the use of cell phones or other recording devices, and extraneous socialization are typically prohibited in dissection settings unless specifically preapproved, and in reverence to the deceased.
7. The cadaver is the central focus of interest and attraction and deserves undivided attention from all present. In addition, the inclusion of a projection screen and whiteboard at each table is desirable to better focus on the topics and techniques being presented and discussed.
8. Cadavers deserve sensitivity, respect, and reverence throughout the process. Some institutions engage a chaplain to assist in this objective.
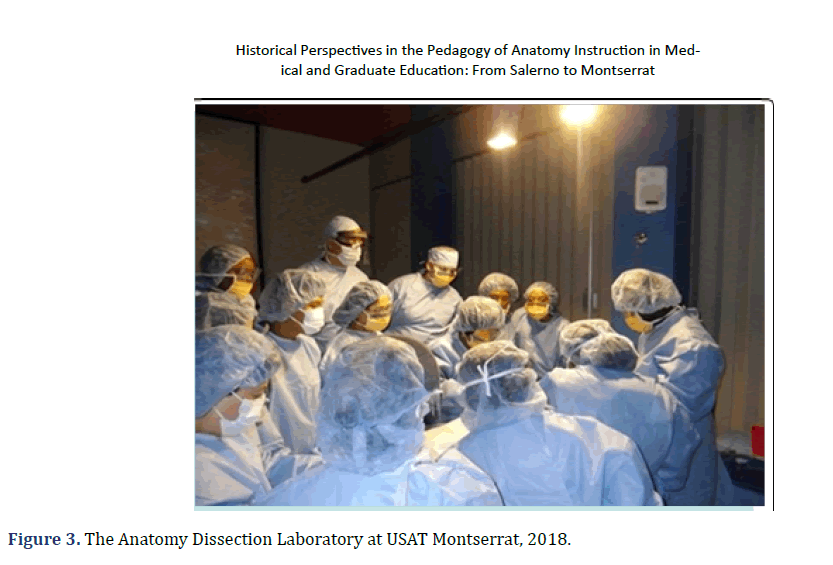
9. Establish a safe and professionally oriented presurgical atmosphere to the dissection exercise, with proper attention to surgical attire and individual demeanor helps to prepare the students for later clinical experiences in a clinical or surgical theater.
10. Upon completion of the laboratory exercise, the student must successfully demonstrate the essential and proper Identification, pathophysiologic functions of each major tissue or organ group.
11. Incorporate clinical examination markers and techniques noting and variations from normal and how one might describe them. Body painting or marking may further enhance this functional aspect of the learning experience for the student.
12. Incorporate additional topics of interest and discussion points such as pathophysiology, endoscopy, bronchoscopy, imaging features, and various types of suturing when and where appropriate and time permitting. Make an attempt to determine the metabolic and pathophysiologic issues present in each cadaveric specimen. Considering the pathology observed, what possible treatments might have been beneficial for this individual as a patient?
13. Upon reaching the endpoint, the student is expected to achieve clinical Competency in Anatomy. Incorporation of new and developing advances in technology of educational pedagogy can present opportunities for change; and when judiciously incorporated, it can fulfill both a need and an opportunity to introduce fresh new insights and Ideas, and to further the discussion of special features that may be discovered in each individual cadaver.
Literature Review
Emerging pedagogy of anatomy and neurobiology instructional methods in the 21st century
The curriculum of anatomy and other courses of medical and graduate instruction underwent progressive revision beginning in 2008 due to the ongoing volcanic activity in Montserrat, in combination with technological improvements in instructional methodology and pedagogy. The advances in instructional technology have been nothing less than remarkable during the past decade with the introduction and development of computer assisted technology assists in higher education. With the continuing development of AI, additional improvements are likely imminent in educational technology applications. As early as 1983, Universities and Colleges began to incorporate computer technology into higher education in the fields of engineering, science, business and in scientific publications with the introduction of the early versions of the Apple and Microsoft platforms [24-30]. Thus the computer era in higher education was well established for many didactic courses before the 21st century, but considerable research and development of computer applications for the study of gross anatomy and its applications to physiology, nutrition, molecular biology, and neurosciences was still in its infancy. But considering that scientific need often paves the road for innovation, emphasis became focused on the more complex nature of the greater detail incumbent in application to studies of Gross anatomy applications at a level consistent with higher level studies in medical education. [ADAM, McIntosh] However, no matter how realistic the computerized versions may become, they have not replaced the physical approach necessary for most surgical applications. The surgeons fine motor coordination and motor skills are paramount to his or her ability to conduct the sophisticated surgical procedures now common in most surgical theaters, and the diagnostic imaging of the practicing radiologist in supporting those invasive procedures with an utmost precision. Moreover, the combined anatomic and imaging skills necessary for many of the computer assisted procedures now commonplace such as tumor ablations, spinal surgeries, and other complex procedures require expertise in both surgical and computer skills by the practicing physician. Thus, the overwhelming need to incorporate the latest in computer applications and surgical finesse are paramount in developing the physicians, surgeons, and biomedical scientists of tomorrow’s surgical theater.
The anatomy dissection program summarized below developed progressively over a period of over 10+ years in advancing to its present state. The program was developed under the oversight of the State-of-the-Art Miami Anatomic Research Center, who made available much of the extensive resources needed to develop the program [31-39]. From the outset, only unembalmed safety tested cadavers were utilized in anatomic dissections and were maintained in a cooled and well-ventilated dissection parlor equipped with well-equipped sanitized, stainless dissection tables for use in active dissection exercises. The use of fresh non-embalmed cadavers is deemed an essential part of the dissection experience as it adds much needed realism to the focus of the laboratory. Stibbs and others have noted that practice interventions with fresh cadavers are more reflective of live tissues than older embalmed cadavers may provide due to the physical nature of the tissues under study, and improve the skill sets of physicians when subjected to similar diagnostic and treatment regimens in a clinical environment at later stages of their training. Thus, the modern-day dissection laboratory is modelled after a surgical theater, complete with availability of imaging devices, surgical instrument trays, fluids and other items and support staff typical of an active surgery centre. Unlike the student lab coats adorned by the participants in past generations, complete PPE, surgical attire, whiteboard and projection screen, and appropriate demeanor is not only deemed essential for instructional purposes in the current educational environment, but for safety concerns as well.
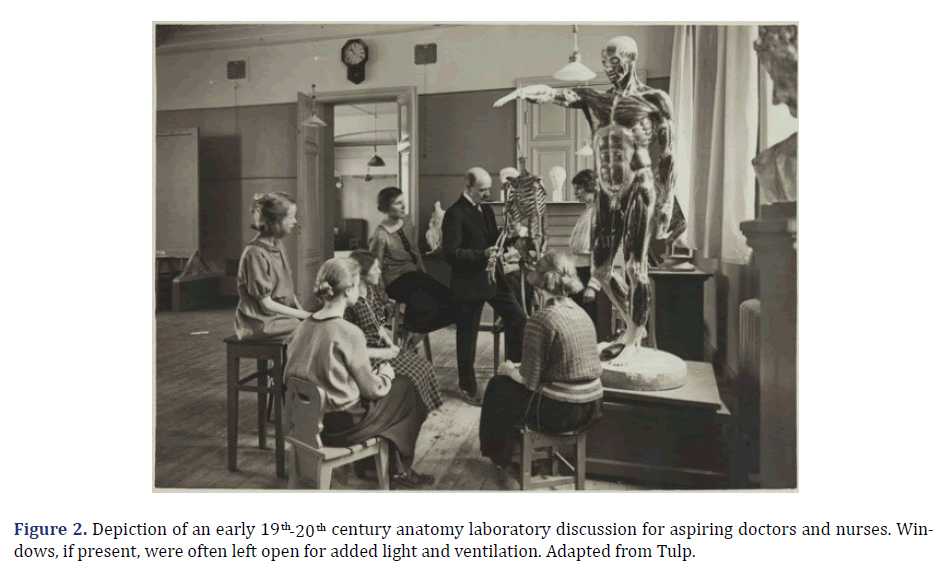
Prior to the onset of each laboratory session, proper respect was offered for the cadaver. (Prior to the dissection instruction, students received training on an Anatomage® table as part of their didactic anatomy lecture course, depicted in Figure. 2.)
In Figure 1, a rendition of Rembrandt’s painting of ‘The Anatomy Lesson of Dr. Tulip’ the renowned Dutch anatomist is depicted and in Figure 2, typical anatomy laboratory of the 19th early 20th century is shown. These figures are contrasted with the current instructional dissection model at USAT depicted in Figure 3. Note the attentiveness to the subject detail in each figure, where a detailed dissection is shown in Figures 1,2 the instructor is pointing out specific important anatomic details deemed important for his discussion. In figure 3, a unique pathologic anatomic finding has been identified and presented on the screen nearby for all to visualize, and positioned such that all students may be called to observe and discuss the uniqueness of the finding.
In Figure 2, when unique or remarkable findings such as depicted here are discovered during a dissection, the participants of all tables can join in the observation, dissection and discussions pertaining to the anatomic findings and treatment plans clinical outcomes.
In Figure 2, a typical anatomy class of the 19th and early 20th century is depicted. In this depiction, students assemble around anatomic models and are shown key structures with their major functions described by the instructor. Such instruction often preceded cadaveric prosection or cadaveric dissection in an adjacent area of the laboratory. Beyond the presentations with anatomic models, the remaining elements of anatomy lab were often an unpopular subject for many students. The twice weekly sessions lab often lasted for up to three semesters, for a minimum of 160 or more total hours in the lab with formalin-embalmed cadavers nearby. PPE or surgical gowns were not provided, at most a student might be assigned or wear a typical lab coat and proceed without surgical gloves. We all remember the unpleasant auras that often followed us around after leaving the lab, and which odors did not improve but became worse as the semester dragged on. Because dissection laboratories were often in the basement level of the buildings which helped to keep the cadavers cooler and away from public view. Windows, if present, might be left open to improve air quality. Laminar flow ventilation in anatomy labs was not yet an option and the potential health risks of formaldehyde exposure on the students were unknown [40].
A typical group of USAT students is depicted in (Figure 3]), the group are participating in a mentored cadaveric dissection, during which all participants cooperate and given the opportunity to take an active part in the dissection process, some as the dissecting surgeon, some in the first assistant role. Each dissection table is planned for up to 6 to 8 students but can accommodate a maximum of 10 to 12 students, including standing platforms in the event they need to look over the shoulders of another student for better viewing. With this approach, procedures may include demonstration of a cardiac massage, dye-enhanced visualization of the coronary arteries prior to further dissection of the heart, again with maximum student participation in process and discussions. It was not uncommon for the students to visualize and palpate an occluded vessel with this technic. Additional procedures including endoscopy or bronchoscopy may be performed during the first phase of the dissection process when the cadaver is deemed suitable for such investigation.
The application of the Anatomage® virtual anatomy is depicted in (Figure 4). In this figure, the images are also shown on the larger screen adjacent to the Anatomage® table. Because both students and faculty can manipulate the images and can confirm the prerecorded identity of the structures depicted to provide immediate feedback this can further enhance the importance and retention of the content of the modules and topics under discussion. In addition, students can return to the Anatomage® table for audit, follow-up, and reinforcement throughout their basic science and clinical years to further reinforce the interrelationships between anatomic structures and their physiologic functions.
Discussion
Additional lab exercises include 3-D printing of body parts, endoscopy, Bronchoscopy, colonoscopy, wound closure and suturing techniques, and others, where a substantial volume of pathophysiology may be discovered during the course of a cadaveric examination and dissection. Overall, the mastery of staged anatomic instruction enables students to better appreciate and reinforce the clinical manifestations of the anatomy, physiology, and neurobiology with carryover to the clinical years and beyond. Anatomy teaching hours have become significantly compressed in recent years to yield room for additional topics in molecular biology and numerous other topics now included in medical basic sciences, many of which have a connection to basic functional anatomy. As a likely result of the innovative emphasis placed on this and other topics during medical basic sciences, student test scores on the basic sciences and clinical sciences pre-licensing examinations have trended upwards with virtually all applicants finding success in their pursuit of postgraduate residency training in the USA and other nations. Because of the above cadaveric dissection program, the previously once somewhat unpopular course of the past has become one of the most popular course modules in the medical basic sciences, with many students requesting the opportunity to audit the module multiple times after their initial experience. Will they become future anatomists or surgeons? Only time may answer that question.
Conclusion
An innovative clinically focused cadaveric anatomy program is described. This program includes traditional didactic, virtual, and specialized cadaveric dissection and has improved the delivery and content retention of anatomy education for medical and graduate students and has become one of the most sought-after modules in the revised and updated curriculum. Clearly, your grandparent’s anatomy lab has left the building and is not here anymore and is unlikely to return in its earlier format, but it hasn’t gone out entirely with the discarded debris, as the fundamental importance of anatomy dissection to medical education remains. Although grandad’s lab it is not likely to return any time soon in its earlier format, the fundamentals, importance and need for mastery of the instruction in gross anatomy remain solid and committed and haven’t changed over the intervening generations. The early process has provided the fundamental basis developed over hundreds of years, since Dr. Nicholaes Tulp’s early demonstration of human dissection as artistically recorded in the ‘Anatomy Lesson of Dr. Tulp’ (ca 1632). Today’s anatomy dissection and modularized learning programs, including computer assisted virtual anatomy programs for human and animal anatomic study via a blended- SPOC (Small Platform Online Course) format now enable and facilitate anatomy instruction to be more meaningful and longer lasting than ever before.
The old adage that stated, “necessity is the mother of invention” likely rings as true in today’s environment as it was in previous generations.
Some aspects of ‘how it was…’ are still important in current pedagogy of medical education. Increasing pressures to improve the efficiency and outcomes of laboratory exercises continue, but now assisted with new and developing technology in the form of virtual anatomy, biophysics, fiberoptics, and electronic media applications. One can simulate neurophysiologic and biophysical phenomenon with predictive accuracy at the molecular level and apply fiberoptic visualizations and 3-D printing exercises not previously adaptable to the anatomy laboratory to supplement the age-old dissecting instruments of yesterday’s lab. This may include computer assisted photography, radiographic imaging, introduction to surgical techniques and procedures, all focused on better preparing the student of today for the clinical experience and demands of tomorrow. Neurophysiologic and biochemical pathways can be modeled, and virtual dose related pharmacologic alterations predicted. In small group discussions, students can discover the uniqueness of each cadaver, relate them to live situations and examples, and engage in healthy and productive discussion with the participating faculty and in attendance, and with computer assisted library resources available as needed. The anatomy laboratory of the 21st century is an evolving program, which will continue to evolve and develop as technology advances and will continue to present an exciting and dynamic opportunity for tomorrow’s medical students to not only master the skills for today but to build on and to develop the skills for a stronger tomorrow. No single approach by itself is likely to be as effective in developing the intellectual and motor skills for future clinical practice as the combined approach using new and developing multimedia and AI-linked approaches. Thus, development of an innovative clinically focused cadaveric anatomy program is described which has improved the delivery and content retention of medical and graduate students and has become one of the most sought-after modules in the updated and revised clinically oriented curriculum.
Acknowledgments
The authors are grateful for the assistance of the many faculty and staff of the Miami Anatomic Research Institute for support and assistance in developing the above program for anatomy dissection for USAT medical students, many of whom entered the program with advanced certifications and degrees, seeking career advancement in the medical professions. Special thanks for the late Dr. David Karam, whose dynamic lecture and brilliant surgical dissection talents were an inspiration to many of his students and to the writing of this manuscript.
Competing Interests
Authors have declared that no competing interests exist.
References
- Hunter M. Alder Hey report condemns doctors, management, and coroner. BMJ 2001;322(7281):255.
[Crossref] [Google Scholar] [Pubmed]
- Bergman EM, Prince KJ, Drukker J, van der Vleuten CP, Scherpbier AJ. How much anatomy is enough? Anat Sci Educ 2008;1(4):184-188.
[Crossref] [Google Scholar] [Pubmed]
- Craig S, Tait N, Boers D, Mcandrew D. Review of anatomy education in Australian and New Zealand medical schools. ANZ J Surg 2010;80(4):212-216.
[Crossref] [Google Scholar] [Pubmed]
- Older J. Anatomy: A must for teaching the next generation. Surgeon 2004;2(2):79-90. [Crossref]
[Google Scholar] [Pubmed]
- Grauer AL, editor. Bodies of evidence: Reconstructing history through skeletal analysis. John Wiley and Sons 1995.
- Hodge CJ. Non-bodies of knowledge: Anatomized remains from the Holden Chapel collection, Harvard University. J Soc Archaeol 2013;13(1):122-149.
- Blakely RL, Harrington JM. Grave consequences: The opportunistic procurement of cadavers at the medical college of Georgia. Bones in the basement: Postmortem racism in nineteenth-century medical training. 1997:162-183.
- Alder Hey report condemns doctors, management, and coroner
- Drake RL, Mcbride JM, Lachman N, Pawlina W. Medical education in the anatomical sciences: The winds of change continue to blow. Anat Sci Educ 2009;2(6):253-259.
[Crossref] [Google Scholar] [Pubmed]
- Bowsher D. What should be taught in anatomy? Med Educ 1976;10(2):132-134.
[Crossref] [Google Scholar] [Pubmed]
- Louw G, Eizenberg N, Carmichael SW. The place of anatomy in medical education: AMEE Guide no 41. Med Teach 2009;31(5):373-386.
[Crossref] [Google Scholar] [Pubmed]
- Ang ET, Sugand K, Hartman M, Seow CS, Bay BH, Abrahams P. Singapore's anatomical future: Quo Vadis? Anat Sci Educ 2012;5(4):234-240.
[Crossref] [Google Scholar] [Pubmed]
- Habicht JL, Kiessling C, Winkelmann A. Bodies for anatomy education in medical schools: An overview of the sources of cadavers worldwide. Acad Med 2018;93(9):1293.
[Crossref] [Google Scholar] [Pubmed]
- Periya SN. Teaching human anatomy in the medical curriculum: A trend review. Int J Adv Res 2017;5(4):445-448.
- Smith C. Water, water everywhere: The pandemic has caused a shortage of cadavers. Britain 2021, edition.
- Shiffer CD, Boulet JR, Cover LL, Pinsky WW. Advancing the quality of medical education worldwide: ECFMG's 2023 medical school accreditation requirement. J Med Regul 2019;105(4):8-16.
- Tulp OL, Ortiz‐Bustillo ML, Einstein GP, Sainvil F, Konyk CM, Branly RL, et al. Innovation in functional anatomy education: The Anatomy Lesson of Dr Tulp from the past to the Present. FASEB J 2018; 32:505.4.
- Tulp OL, Sainvil F, Einstein GP, Sciranka A, Branly R, Wu H, et al. Incorporation of virtual enhancement in anatomy, physiology and clinical pathology instruction in medicine and veterinary medicine basic sciences. FASEB J 2022;36.
- Tulp O, Sainvil F, Wu H, Feleke Y, Einstein G, Branly R. Modernization of Anatomy and Graduate Medical Education from the Past to the Present. FASEB J 2021;35.
- Leung KK, Lu KS, Huang TS, Hsieh BS. Anatomy instruction in medical schools: Connecting the past and the future. Adv Health Sci Educ Theory Pract 2006; 11:209-215.
[Crossref] [Google Scholar] [Pubmed]
- Anastakis DJ, Regehr G, Reznick RK, Cusimano M, Murnaghan J, Brown M, et al. Assessment of technical skills transfer from the bench training model to the human model. The Am J Surg 1999;177(2):167-170.
[Crossref] [Google Scholar] [Pubmed]
- Keim Janssen SA, Vandermeulen SP, Shostrom VK, Lomneth CS. Enhancement of anatomical learning and developing clinical competence of first‐year medical and allied health profession students. Anat Sci Educ 2014;7(3):181-190.
[Crossref] [Google Scholar] [Pubmed]
- Anyanwu EG, Obikili EN, Agu AU. The dissection room experience: A factor in the choice of organ and whole body donation-A Nigerian survey. Anat Sci Educ 2014;7(1):56-63.
[Crossref] [Google Scholar] [Pubmed]
- Kalanjati VP, Prasetiowati L, Alimsardjono H. The use of lower formalin-containing embalming solution for anatomy cadaver preparation. Med J Indones 2012;21(4):203-207.
- Whitehead MC, Savoia MC. Evaluation of methods to reduce formaldehyde levels of cadavers in the dissection laboratory. Clin Anat 2008;21(1):75-81.
[Crossref] [Google Scholar] [Pubmed]
- Ocel JJ, Natt N, Tiegs RD, Arora AS. Formal procedural skills training using a fresh frozen cadaver model: A pilot study. Clin Anat. 2006;19(2):142-146.
[Crossref] [Google Scholar] [Pubmed]
- Prasad N, Kumar S, Manjunath R, Bhadauria D, Kaul A, Sharma RK, et al. Real-time ultrasound-guided percutaneous renal biopsy with needle guide by nephrologists decreases post-biopsy complications. Clin Kidney J. 2015;8(2):151-156.
[Crossref] [Google Scholar] [Pubmed]
- Reed AB, Crafton C, Giglia JS, Hutto JD. Back to basics: Use of fresh cadavers in vascular surgery training. Surgery 2009;146(4):757-763.
[Crossref] [Google Scholar] [Pubmed]
- Are C, Lomneth C, Stoddard H, Azarow K, Thompson JS. A preliminary review of a pilot curriculum to teach open surgical skills during general surgery residency with initial feedback. Am J Surg 2012;204(1):103-109.
[Crossref] [Google Scholar] [Pubmed]
- Meek ME, Meek JC, Hollowoa B, Li R, Deloney LA, Phelan KD. Lightly embalmed cadavers as a training tool for ultrasound-guided procedures commonly used in interventional radiology. Acad Radiol 2018;25(11):1503-1509.
[Crossref] [Google Scholar] [Pubmed]
- Hoyer R, Means R, Robertson J, Rappaport D, Schmier C, Jones T, et al. Ultrasound-guided procedures in medical education: A fresh look at cadavers. Intern Emerg Med 2016; 11:431-436.
[Crossref] [Google Scholar] [Pubmed]
- Asad MR, Nasir N. Role of living and surface anatomy in current trends of medical education. Int J Adv Res Innov Ideas Educ 2015;1:203-210.
- Finn GM. Twelve tips for running a successful body painting teaching session. Med Teach 2010;32(11):887-890.
[Crossref] [Google Scholar] [Pubmed]
- Finn GM, Mclachlan JC. A qualitative study of student responses to body painting. Anat Sci Educ 2010;3(1):33-38.
[Crossref] [Google Scholar] [Pubmed]
- Nanjundaiah K, Chowdapurkar S. Body-painting: A tool which can be used to teach surface anatomy. J Clin Diagn Res 2012;6(8):1405.
[Crossref] [Google Scholar] [Pubmed]
- Collett T, Kirvell D, Nakorn A, Mclachlan JC. The role of living models in the teaching of surface anatomy: Some experiences from a UK Medical School. Med Teach 2009;31(3):e90-e96.
[Crossref] [Google Scholar] [Pubmed]
- Bickley LS, Szilagyi PG, Hoffman RM, Soriano RP. In: Bate’s Guide to Physical Examination and History taking. 13th edn. Lippincott Pubs. 2020.
- Hoyek N, Collet C, di Rienzo F, de Almeida M, Guillot A. Effectiveness of three‐dimensional digital animation in teaching human anatomy in an authentic classroom context. Anat Sci Educ 2014;7(6):430-437. [Crossref]
[Google Scholar] [Pubmed]
- Tulp OL. Enhancing the pedagogy of global medical education with a blended SPOC program: The anatomy lesson of Dr. Nicholaes Tulp revisited. Presented at the 4th International Conference on Vaccine Research/Global Medical Education, UK Conference Series, Madrid, Spain, February 8-9, 2024.
- Tulp OL. Observations of the introduction of the personal computer to academia at Drexel University. 1983-1984.