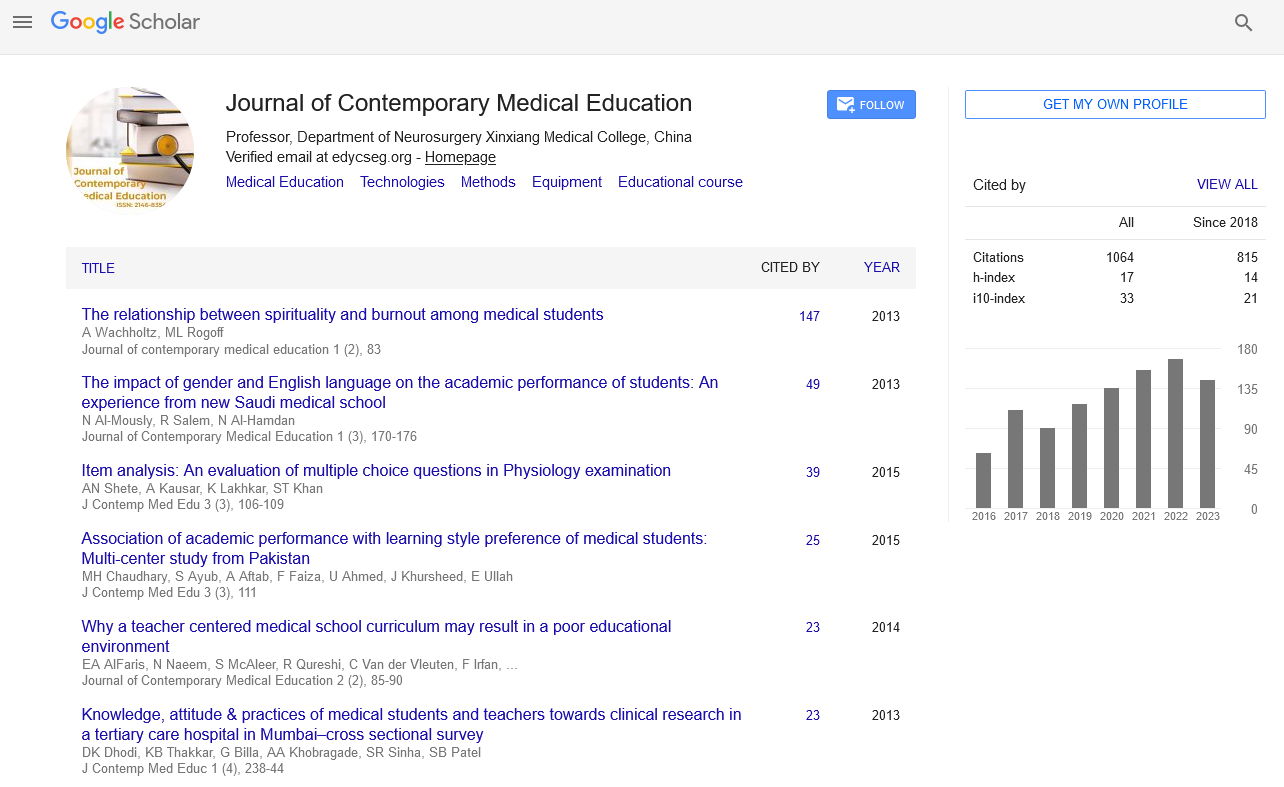
Perspective - Journal of Contemporary Medical Education (2023)
Complexities of Guillain Barre Syndrome: Evolving Strategies for Treatment and Therapeutic Interventions
Sohan Malik*Sohan Malik, Department of Medicine, University of Chicago, Chicago, USA, Email: Sohanmalik@gmail.com
Received: 04-Oct-2023, Manuscript No. JCMEDU-23-121758 ; Editor assigned: 09-Oct-2023, Pre QC No. JCMEDU-23-121758 (PQ); Reviewed: 23-Oct-2023, QC No. JCMEDU-23-121758 ; Revised: 30-Oct-2023, Manuscript No. JCMEDU-23-121758 (R); Published: 06-Nov-2023
Description
Guillain Barre syndrome (GBS) is a rare but serious autoimmune disorder characterized by the body's immune system mistakenly attacking the peripheral nerves. This condition leads to nerve inflammation, causing muscle weakness, numbness, and in severe cases paralysis. GBS typically begins with tingling sensations and weakness in the legs, often spreading to the arms and upper body. It can progress rapidly, leading to varying degrees of muscle weakness or paralysis. The exact cause of GBS is not fully understood, but it often follows infections, such as respiratory or gastrointestinal infections or can be associated with vaccinations or surgery, although these occurrences are relatively rare.
Symptoms
GBS typically starts with tingling sensations and weakness in the legs, often spreading upward to the arms and upper body. Symptoms can progress rapidly, causing muscle weakness or paralysis. Common signs and symptoms include:
Tingling or numbness: Often starting in the feet or hands and spreading.
Muscle weakness: Usually beginning in the legs and progressing to the upper body, potentially causing difficulty moving, swallowing, or speaking.
Pain: Some individuals may experience severe pain, especially in the back and legs.
Difficulty breathing: In severe cases, weakness in respiratory muscles can lead to breathing difficulties requiring medical intervention.
Causes
The exact cause of GBS is not fully understood, but it's believed to be an autoimmune response triggered by infections or other factors. Potential causes and contributing factors include:
Infections: GBS often follows an infection, most commonly caused by bacteria or viruses. Respiratory or gastrointestinal infections, such as those from campylobacter jejuni, Cyto Megalo Virus (CMV), or the Epstein-Barr virus (EBV), are often associated with GBS.
Vaccinations: In rare cases, certain vaccinations, particularly the flu vaccine and the vaccine for the Zika virus, have been linked to GBS.
Surgery: GBS may occur after surgery or trauma, although these instances are relatively rare.
Risk factors
While GBS can affect anyone, several factors may increase the risk of developing this condition:
Age and gender: GBS can occur at any age, but it's slightly more common in adults and males.
Infections: Recent infections, particularly those caused by campylobacter jejuni, increase the risk of GBS.
Previous occurrences: Having had GBS in the past slightly increases the risk of a recurrence.
Complications
In severe cases, GBS can lead to life-threatening complications, such as breathing difficulties or cardiac problems. However, many individuals recover partially or fully with appropriate treatment. Recovery from GBS can be slow and may involve rehabilitation, physical therapy, or occupational therapy to regain strength and mobility. GBS is a rare but serious neurological disorder characterized by the immune system attacking peripheral nerves. Its sudden onset and potential severity necessitate prompt medical attention. While much remains to be understood about its exact causes and mechanisms, early recognition, accurate diagnosis, and timely intervention are vital for managing GBS and achieving the best possible outcomes for affected individuals. Ongoing research aims to improve patient understanding of this complex condition and develop more effective treatments.
Diagnosis and treatment
Diagnosing GBS often involves a combination of medical history, physical examination, and tests, including nerve conduction studies and lumbar puncture (spinal tap) to analyze cerebrospinal fluid. Treatment for GBS focuses on managing symptoms and preventing complications. Intravenous Immunoglobulin (IVIG) therapy, which involves infusions of healthy antibodies, and plasmapheresis, a procedure to remove harmful antibodies from the blood, are common treatments to reduce the severity and duration of the illness.