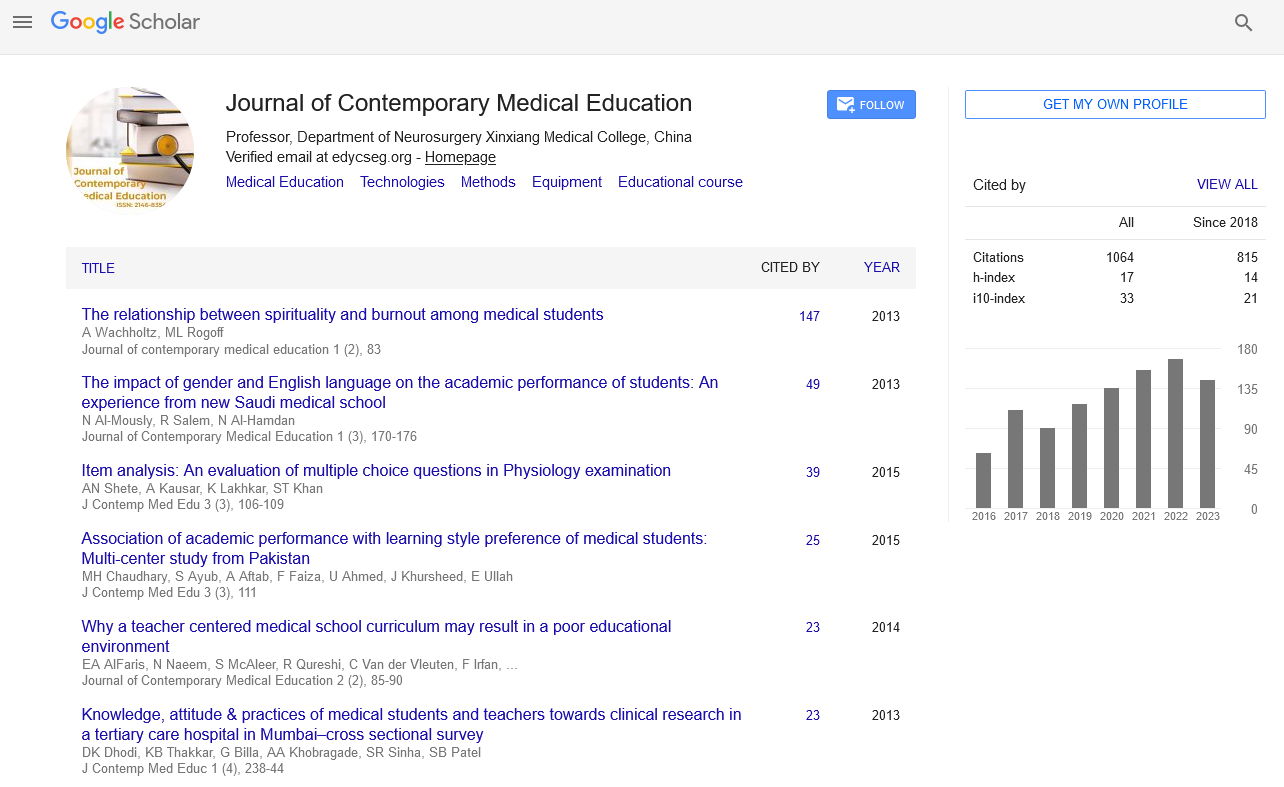
Research Article - Journal of Contemporary Medical Education (2021)
A Novel Remote Induction Programme for New Junior Doctors during the COVID-19 Pandemic
Sean Lobo*, Mostafa Khalil, Wen Ling Choong and John ScollaySean Lobo, Department of General Surgery, Ninewells Hospital, United Kingdom, Email: seanlobo95@outlook.com
Received: 18-Aug-2021 Published: 08-Sep-2021
Abstract
Introduction: Starting a new job as a junior doctor is often challenging. In addition, doctors who have recently commenced employment have been impacted by the COVID-19 pandemic. This has affected them in multitude of detrimental ways, including reduced clinical exposure for final year medical students, as well as, hampering the traditional face to face clinical induction.
Methods: To help foundation doctors who were starting work during the pandemic, we developed an additional trainee led and facilitated remote induction programme. This consisted of a series of online sessions, covering areas such as prescribing, management of the acutely unwell patient and effective organisation/prioritisation. We utilized a number of different techniques, including virtual simulations to ensure engagement and interactivity. Prior to the commencement of the programme, we measured the confidence of participants across several parameters including managing unwell patients, prescribing, and dealing with nightshifts. The same parameters were re-assessed following completion of our programme.
Results: Following completion of our course we noted a trend towards improvement in the self-reported confidence scores across all parameters. The greatest improvement was noted in “management of the acutely unwell patient”, with scores increasing from 4.074 ± 0.522 to 6.00 ± 0.503 after completion of the programme.
Discussion: Completion of our remote induction programme has helped new foundation doctors improve their confidence in dealing with common clinical scenarios and potentially improved prescribing practice. A trainee led/facilitated remote induction programme has many advantages.
Keywords
Clinical induction; COVID-19 pandemic; Survey monkey; Clinical work
Introduction
Starting a new job as a junior doctor is often challenging, particularly on surgical wards, as patients are often acutely unwell. The 2020 intake of junior doctors faced an additional challenge they had started work during the COVID-19 pandemic, which affected these new clinicians in a multitude of detrimental ways [1].
It has been previously suggested that there is an increase in mortality when there is a junior doctor changeover, with figures of 4%-12% being quoted. This has led to terms such as the ‘August Effect’ or ‘Black Wednesday’ [2]. It has been suggested that an effective induction programme can help improve patient safety and the confidence of new clinicians [3].
The COVID-19 pandemic has challenged how a traditional induction programme can be effectively delivered. Issues have included social distancing requirements and the potential for doctors to miss a conventional face to face session if they were unwell with COVID-19 or required to self-isolate. This problem is further compounded when one considers that these new doctors will have had no experience of COVID related practice and an induction event is the ideal forum to explain protocols relating to patient management, infection control and workplace behaviour.
We set out to develop and implement an effective remote induction programme to improve junior doctors’ confidence by equipping them with the requisite skillset to thrive in the clinical environment. It was intended that this additional programme would be complementary to the mandatory hospital induction. In addition, it was desired that these additional sessions would be trainee led and delivered by trainee doctors of varying grades.
When developing this programme, we considered the challenges medical students face when transitioning to the role of a doctor. These included a steep learning curve relating to clinical practice, the need to develop team working skills and the requirement to be able to ask for clinical or pastoral help [4]. Bearing in mind these themes, we developed a virtual induction programme utilising a range of educational modalities and with contributions from a multidisciplinary professional team.
Methods
The induction programme consisted of a series of online interactive tutorials. These sessions were offered to a cohort of new foundation doctors who were starting work in a large surgical department in a UK teaching hospital. These new doctors were commencing placements in General Surgery, Urology, and Vascular Surgery (with an expectation they would cross cover between these specialties).
Each educational session was tailored to allow development and learning in a specific area of clinical practice. The programme was delivered between August 2020 and November 2020. Surgical foundation doctors, who had recently commenced their training, were invited through emails, word of mouth and social media.
Prior to each session, a survey was circulated to all potential participants to determine their confidence and knowledge regarding the upcoming topic (Table 1). These surveys were circulated utilizing Survey Monkey (an online platform designed to deliver surveys and obtain anonymous feedback). At the time of completing this initial survey participants were given the opportunity to raise specific questions that they wished answered during the online tutorial.
| Survey Questions (pre 1st Session) | |
| On a scale of 1-10 how confident are you on the surgical wards | |
| Please comment below (what you feel confident in, what you are worried about) | |
| On a scale of 1-10 how confident are you in prescribing | |
| What specifically concerns you about prescribing? | |
| Survey Questions (pre 2nd Session) | |
| On a scale of 1-10 How confident are you in dealing with an acutely unwell patient? | |
| Please comment below (what you feel confident in, what you are worried about) | |
| On a scale of 1-10 How confident are you seeing patients alone? | |
| What specifically concerns you about seeing patients independently? | |
| Do you stay on top of jobs as they are given to you? | |
| Are you confident in prioritizing jobs by clinical need? | |
| Survey Questions (pre 3rd Session) | |
| How confident do you feel on a Night Shift on a scale of 1-10 (10=most confident) | |
| What worries you about Night Shift? | |
| Do you feel supported on a night shift | |
| Do you know what is expected of you during a night shift? | |
| Survey Questions (pre final Session) | |
| On a scale of 1-10 how well do you feel you keep organized and on top of jobs? | |
| On a scale of 1-10 how well do you prioritize tasks and patients? | |
| Do you feel you know at what point to escalate to seniors? | |
| Do you have any specific questions or topics to be covered? |
All online induction sessions were provided via Zoom video conferencing technology. Permission was sought to record each session so doctors not present could review the material later.
The first session focused on prescribing and was led by a specialist surgical pharmacist, who provided an interactive lecture. During the session, the pharmacist demonstrated real life anonymised medical prescription errors. At the end of the session, resources were circulated which provided guidance about common prescribing scenarios that the participants had highlighted, or that the pharmacist felt were particularly relevant to foundation doctors.
The second module was led by a senior surgical registrar and concentrated on the management of acutely unwell patients. The doctor gave description of clinical situations they had encountered during their clinical practice and facilitated group discussion of these scenarios. This session was intended to ensure that doctors could develop a set framework to systemically assess each patient and ensure clinically safe and appropriate actions. To help ensure the session was interactive and immersive real life observation charts and drug charts were utilized (Figure 1). This session was intended to demonstrate that an emergency generic management is often more important than determining an exact diagnosis. Foundation doctors were able to make suggestions and subsequently reflect on their ideas in a supervised environment whilst also being able to critically analyze the alternative strategies suggested by other participants.
The third session covered working as junior doctor on night shift, as it was identified that the new cohort of junior doctors felt unprepared for night shifts. This was expressed through informal feedback to seniors prior to the programme and was also noted during collection of the surveys initially.
The fourth and final session focused on personal organization and task prioritization. The aim of this session was to assist these new doctors develop into an effective and organized clinician. This tutorial was led by a senior surgical registrar who utilized real life clinical scenarios to demonstrate efficient working practices. In addition, a clinical development fellow offered generic advice regarding time management during periods of ward work.
Following completion of the programme feedback surveys were issued to all participants to assess subjective self-reported improvement in confidence in dealing with the issues covered in the teaching sessions.
Results
This induction programme was offered to 21 of the foundation doctors. Out of these doctors, 14 successfully attended each of the four sessions and completed both the initial and final survey.
Prior and after to the commencement of the project new medical graduates were asked to rate their confidence (on a scale of 1-10) in dealing with the 4 themes covered in the programme. In addition, using a combination of ratings scales and free text responses they were asked to provide other information regarding their concerns about starting work. Following successful completion of the programme participants were asked to re-evaluate their confidence in dealing with these themes.
The results of the pre and post programme questionnaires are demonstrated in Table 2. In addition, review of the free text responses revealed some common concerns.
| Survey Questions (pre 1st Session) | Average (mean) Value before session (confidence interval to 95%) | Average (mean) Value at the end of the teaching programme (confidenceinterval to 95%) |
|---|---|---|
| On a scale of 1-10 how confident are you on the surgical wards | 4.5 ± 0.733 STD 1.40 | 5.92 ± 0.561 STD 1.072 |
| Please comment below (what you feel confident in, what you are worried about) | Variety of patients Seniors may be in theatre | Seniors may be in theatre |
| On a scale of 1-10 how confident are you in prescribing | 5.57 ± 0.673 STD 1.28 | 6.50 ± 0.448 STD 0.854 |
| What specifically concerns you about prescribing? | Unfamiliarity with some drugs Insulin | n/a |
| Survey Questions (pre 2nd Session) | ||
| On a scale of 1-10 How confident are you in dealing with an acutely unwell patient? | 4.07 ± 0.522 STD 0.10 | 6.00 ± 0.503 STD 0.960 |
| Please comment below (what you feel confident in, what you are worried about) | Unpredictability Not confident in own abilities Not sure when to escalate |
Unpredictability |
| On a scale of 1-10 How confident are you seeing patients alone? | 3.64 ± 0.639 STD 1.22 | 5.21 ± 0.828 STD 0.726 |
| What specifically concerns you about seeing patients independently? | Unpredictability Too much responsibility Not sure when to escalate |
unpredictability |
| Do you stay on top of jobs as they are given to you? | 4 Yes/10 No | 7 Yes/7 No |
| Are you confident in prioritising jobs by clinical need? | 9 Yes/5 No | 14 Yes |
| Survey Questions (pre 3rd Session) | ||
| How confident do you feel on a Night Shift on a scale of 1-10 (10=most confident) | 4.71 ± 0.38 STD 0.726 | 6.00 ± 0.822 STD 1.569 |
| What worries you about Night Shift? | unclear role perceived lack of support |
Perceived lack of support Specialties not seen during the day |
| Do you feel supported on a night shift | 8 Yes/6 No | 10 Yes/4 No |
| Do you know what is expected of you during a night shift? | 8 Yes/6 No | 12 Yes/2 No |
| Survey Questions (pre final Session) | ||
| On a scale of 1-10 how well do you feel you keep organised and on top of jobs? | 5.14 ± 0.576 STD 1.10 | 6.21 ± 0.511 STD 0.975 |
| On a scale of 1-10 how well do you prioritise tasks and patients? | 6.00 ± 0.617 STD 1.177 | 7.14 ± 0.4037 STD 0.770 |
| Do you feel you know at what point to escalate to seniors? | 6 Yes/8 No | 14 Yes |
Following completion of the online induction programme we noticed a trend that suggested that new foundation doctors were increasingly confident with the 4 themes covered in our induction programme (Figure 2).
Discussion
The aim of this project was to utilize a number of different modalities to provide an induction programme that equipped FY1 junior doctors to manage common medical issues appropriately on a surgical ward.
We found that the two lowest scoring parameters at the start of the project were confidence in seeing patients alone, and the management of the acutely unwell patients. We identified that these are issues that are often reported to be particularly challenging for junior doctors [5]. Within our team, we sought to equip the new foundation doctors with a generic framework that may be utilized in a variety of acute clinical settings. In an ideal setting, a suitable adjunct would be the utilization of high fidelity simulations, to replicate unwell patients, as simulations have been proven to improve safety and reliability in high stress settings [6]. However, this was limited due to social distancing guidelines. We partially counteracted this by utilizing adjuncts that the junior doctors will encounter in the clinical setting, such as observation charts and prescription charts. At the end of the programme, confidence in management of the acutely unwell patient, reported the highest increase in score following delivery of the programme.
We note that we saw the most minimal increases in the self-reported scores in organization and prioritization of tasks, though these parameters did also have the highest baseline scores. These are skills that some may argue are inherent, or may be developed through active immersion, rather than remote teaching programmes [7]. Nonetheless, an improvement in confidence was still noted in this score, and we believe that this was due to the provision of methods to prioritize tasks and develop organisational skills. Demonstrating frameworks and successful tools to an audience, encourages them to employ it in their future practice to remain organised [8].
To maximize engagement with participants in a teaching programme, a variety of modalities should be employed to hold interest and present information clearly [9]. Therefore, we sought to maximize the variety of topics and presentation techniques utilized. For instance, when undertaking the prescribing teaching session, we used a PowerPoint presentation to highlight local guidelines. To demonstrate correct prescribing methods; we utilized the same paper drug charts encountered in the clinical environment. Furthermore when discussing acute clinical scenarios, we utilized clinical accessories such as observation charts and images of paraphernalia associated with the discussed clinical scenarios. This ensured that we developed familiarity of the clinical environment, enabling the junior doctors to be prepared to encounter these scenarios during their clinical work [10].\
We were also aware of the challenges faced, both in terms of mental and physical fatigue. We ensured to complete these sessions in the early evening to ensure maximum attendance, but we also aimed to ensure that each session was limited to a maximum of one and a half hours to minimize fatigue, and we also ensured that each session had at least one break [11].
The programme took place over a 3 month period. Whilst we may attribute the global improvement in confidence across parameters due to our teaching sessions, there may also be other factors influencing this improvement. The most obvious factor, being that this was the first placement for study participants hence one would expect their baseline confidence to be low, and increase after 3 months of clinical practice [12]. Although this was undoubtedly a confounding factor we believe the programme accelerated the acquisition of skills and confidence [13].
Conclusion
A successful induction programme should address the new doctor’s concerns and expectations, whilst providing with the appropriate framework to develop clinically in a new role or setting. With the advent of the COVID-19 pandemic, this was a challenge to ensure we fulfilled these aims, whilst adhering to national policy on social distancing and other preventative measures. Therefore, we worked with a multidisciplinary team to develop and implement a novel remote induction/teaching programme aimed at new and inexperienced surgical doctors. Following the programme, we noted an improvement in confidence across all parameters. Whilst there may be other factors at play, we suggest some of these improvements were due to the successful delivery of this programme. We noted the success of certain techniques which we will seek to continually employ in induction programmes, whether indicated by a pandemic or not.
Conflict of Interest
The authors declare no conflicts.
References
- Dedeilia A, Sotiropoulos MG, Hanrahan JG, Janga D, Dedeilias P, et al. Medical and surgical education challenges and innovations in the COVID-19 Era: A systematic review. In Vivo. 2020; 34(3 Suppl):1603-1611.
- Gaskell N, Hinton R, Page T, Elvins T, Malin A. Putting an end to black wednesday: Improving patient safety by achieving comprehensive trust induction and mandatory training by day 1. Clin Med. 2016; 16(2): 124–128.
- McCullough J, van Hamel C. Anxiety among newly quali?ed doctors. An 8 year analysis. Med Teach 2020; 42(1):52–57.
- Sturman N, Tan Z, Turner J. A steep learning curve: junior doctor perspectives on the transition from medical student to the health-care workplace. BMC Medical Education. 2017; 17(1).
- Tallentire VR, Smith SE, Skinner J, Cameron HS. Understanding the behaviour of newly qualified doctors in acute care contexts. Medical Education. 2011; 45(10): 995–1005.
- Kurup V, Matei V, Ray J. Role of in situ simulation for training in healthcare. Current Opinion in Anaesthesiology. 2017; 30(6): 755–760.
- Wicker P. Organisational skills and tools. J Perioperative Prac. 2009; 19(4):136–141.
- Matthews JH, Morley GL, Crossley E, Bhanderi S. Teaching leadership: The medical student society model. The Clinical Teacher. 2017; 15(2): 145–150.
- Dyer E, Swartzlander BJ, Gugliucci MR. Using virtual reality in medical education to teach empathy. J Medi Lib Asso. 2018; 106(4): 498–500.
- McGaghie WC, Issenberg SB, Petrusa ER, Scalese RJ. A critical review of simulation- based medical education research: 2003-2009. Medical Education. 2010; 44: 60-63.
- Bisholt B, Ohlsson U, Engström AK, Johansson AS, Gustafsson M. Nursing students' assessment of the learning environment in different clinical settings. Nurse Educ Pract. 2014; 14(3):304–310.
- Lees MC, Zheng B, Daniels LM, White JS. Factors affecting the development of confidence among surgical trainees. J SurgEdu. 2019; 76(3): 674–683.
- Flemming S, Hankir M, Ernestus RI, Seyfried F, Germer CT, et al. Surgery in times of COVID-19 recommendations for hospital and patient management. Langenbeck’s Archives of Surgery. 2020; 405(3): 359–364.