Research Article - Journal of Contemporary Medical Education (2024)
A Curriculum Preparing Tomorrow’s Radiology Educators: A Long-Term Evaluation of Effectiveness
Emad Allam*, Jennifer Lim-Dunham, Alexander Kui and Laurie M LomasneyEmad Allam, Department of Radiology, Loyola University Medical Center, Illinois, USA, Email: Emad.allam@lumc.edu
Received: 14-Mar-2024, Manuscript No. JCMEDU-24-129457; Editor assigned: 19-Mar-2024, Pre QC No. JCMEDU-24-129457 (PQ); Reviewed: 02-Apr-2024, QC No. JCMEDU-24-129457; Revised: 09-Apr-2024, Manuscript No. JCMEDU-24-129457 (R); Published: 16-Apr-2024
Abstract
Background: Medical education programs infrequently provide focused opportunities to develop skills to be an effective educator.
Objective: We provide a description and analysis of a successfully integrated program that builds a foundation for imaging residency trainees to become effective educators.
Methods: A training curriculum with three pillars was developed-electronic presentation development, public speaking best practices, and literature review. This parallel curriculum to Diagnostic Radiology (DR) and Nuclear Medicine (NM) residencies has designated mentors. Following IRB approval, an anonymous electronic survey in Likert scale format was sent in 2022 to 10 program participants and 27 peer-matched trainees to evaluate background training in education, perceived skills/confidence with public presentation, and current practice environment. Semi-quantitative analysis was performed.
Results: 9 (9/10,90%) participants and 15 (15/27,56%) matched trainees responded to the survey. 23 of 24 (96%) respondents had received no prior formal training for teaching prior to access to the program. When ranked on a Likert scale for severity of competition with residency, 9 participants responded no to mild interferences. Regarding self- evaluated personal confidence in presentation skills, program participants scored an average of 4.1, while non-participants scored 3.6, when ranked on a scale of 0 (none) to 5 (extreme). While 6/6 (100%) graduate program respondents indicated ongoing roles in education, only 3/11 (27%) non-program graduates contributed.
Conclusion: This longitudinal curriculum functions parallel to formal imaging residencies offering residents an opportunity to learn effective skills for teaching. This program may enhance both personal career satisfaction and expertise of our future educators.
Keywords
Radiology; Educator; Curriculum; Training; Skills
Introduction
Training to be a physician is a grueling task, requiring years of intellectual and emotional commitment to acquire the knowledge and skills to care for patients. However, many of the young graduate colleagues will transition to an additional role-educator. Since training programs traditionally provide little or no support for their development as a teacher, a motivated trainee will have to identify potential learning resources on their own. Literature is one potential resource [1,2]. Virtual lectures, such as TED talks, provide an abundance of examples and tricks [3]. Technical aids and on-line support systems for specific presentation platforms can be useful. An integrated program that consolidates the salient points and basic technical skills of a successful presentation would be essential to providing a base on which to build an academic career. This manuscript reviews and analyzes the program we have developed, the Pathway for Added Certification in Education (PACE), to build skills important for effective public presentation with careful consideration of the impact on residency training.
Materials and Methods
The PACE curriculum is completed by selected trainees over 2 (NM) or 2-3 (DR) years. The various activities and tasks of the PACE program revolve around three basic elements-computer based technical presentation, personal presentation, and theoretical principles of education. Activities (lectures, presentations, tasks) were scheduled specifically to the individual participant’s imaging training program schedule.
PowerPoint (Microsoft) presentation is emphasized [4]. The basic skills of participants are refined to ad- dress unique tactics for presenting imaging findings such as utilization of a dark background to preserve retinal detail, compressing images to remove private data, and employing morphing from large Field-Of-View (FOV) to minimized FOV for emphasis. For versatility, at least one new presentation format (such as Prezi) is explored. Trainees give presentations requiring increasingly complex program applications; critiques by mentors identify best practices and opportunities for improvement..
The curriculum also emphasizes the physical aspects of presentation (stance, body language, verbal speech) through group sessions. Participants learn to identify their target audience and define what tactics would enhance the probability of success in reaching learners and buying confidence in a short time span. Concepts of facing the audience, using open hand gestures, speaking with confidence are all emphasized. Skills are reinforced with presentations; feedback follows completed presentations.
Literature on information processing and retention is explored to establish a scientific understanding of teaching and learning. Tactics applicable to tailoring presentation tactics for maximum receptivity and retention of the adult-learner audience are reviewed. A stock library is utilized, in addition to resident-selected resources shared in a reverse-classroom format. Guest lecturers from the local Graduate Medical Education Office and other institutional subspeciality departments provide additional perspectives.
Various venues are used to gain confidence and mastery of skills. PACE trainees act as technical support for medical students, guiding them through or moderating their presentations. Program participants provide a minimum of four presentations for resident trainees and/or medical students. In the last year of training, PACE participants complete a PACE rotation for skill/ knowledge consolidation. The trainee is expected to develop a new teaching tool/resource for other learners, with sustainability a key expectation. Cost of the program is realized in time on the part of mentors and participants.
Following IRB approval (informed consent waived), in 2022, 10 program participants and 27 peer matched non-participant trainees were sent anonymous electronic surveys developed at this institution via Microsoft Outlook Forms. The survey included 14 questions for non-PACE participants and 28 questions for PACE participants (Appendix). Questions from the survey included background information (prior training in the processes of education, level of confidence in presentation/teaching skills, current practice environment) as well as information specific to the program (competition with res- idency training, quality of program components, perceived benefits to personal education). Respondents completed the surveys as a ranked Likert scale ranging from 0-5 (0-Strongly Disagree; 5-Strongly Agree). Returned surveys were evaluated with comparison of results between participant and non-participant cohorts for identification of trends.
Results
At the time of analysis, there were 10 active or graduated participants of the education program. No participants have withdrawn or been prematurely released from the program. All graduate participants have successfully graduated from their respective Nuclear Medicine (2) and Diagnostic Radiology (5) training programs, or they are currently enrolled in good standing (3). 9/10 participants (90%) (3 current program participants) and 15/27 (56%) non-participants responded to the survey.
Survey results showed that 23 of 24 (96%) respondents had received no prior formal training in the processes of learning and education during their medical training. Survey anonymity precludes identification of the one individual with training, but at best, this would indicate that 8/9 (89%) PACE participants had not received prior focused training. All PACE respondents indicated perceived benefits for developing important skills from the program in general, specifically indicating the technical components as the most useful. All PACE respondents would recommend the program.
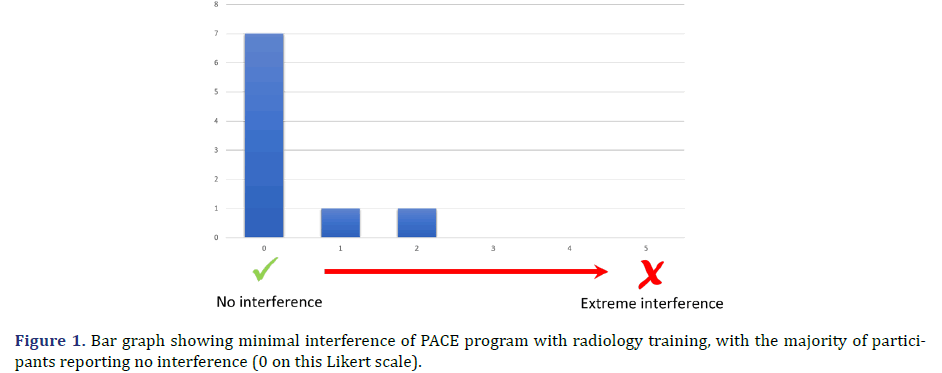
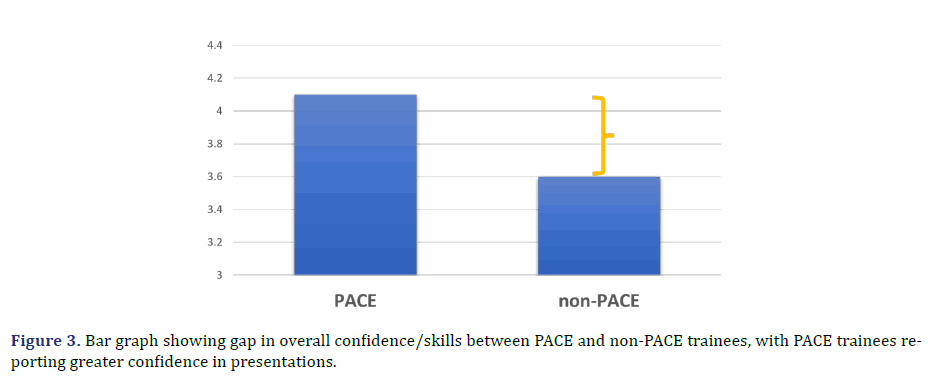
When ranked on a Likert scale of 0 (none) to 5 (extreme) for severity of competition with the imaging training program, 7/9 (78%) of program participants responded no interferences, with the remaining two respondents indicating a rank of 1 or 2 (minimal or mild interference) (Figure 1). Survey participants were asked to self-evaluate personal confidence in presentation skills. When ranked on a scale of 0 (none) to 5 (extreme), PACE respondents had an average score of 4.1 while non-PACE participants had an average score of 3.6 (Figure 2).
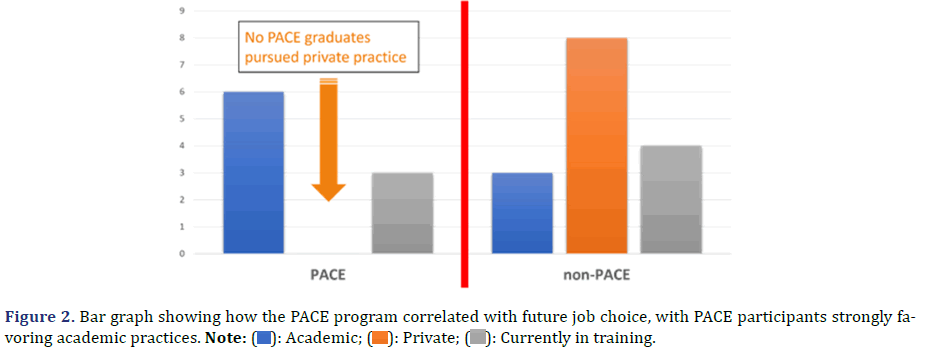
When comparing job practices of graduates, 6/6 (100%) PACE graduates currently practice in an academic environment whereas 8/11 (73%) non-PACE graduates practice in a private environment (Figure 3). Since educational roles can blur between practice environments, graduate respondents were also asked about current involvement in medical education. While 6/6 (100%) graduate PACE respondents indicated ongoing roles in education, only 3/11 (27%) non-PACE graduates contributed.
Discussion
Although teaching is an inherent component of an academic faculty appointment, most training programs lack defined curricula that give residents opportunities to develop the necessary skills to perform optimally as an educator. A structured integrated training program for resident trainees supports both skill level and confidence for providing medical education.
Characteristically, trainees (residents and fellows) find themselves transitioning to the title of ‘educator’ based on date of graduation rather than skill set [5]. There are a few individual residency training programs that offer teaching experiences, with a variety of approaches such as focused independent training as a peer educator or a month-long rotation in the clinical block [6,7]. Some academic institutions offer independent training courses separate from the residency training, including opportunities for a master’s degree [8,9]. Especially apropos in our current remote learning environment, there is also an online curriculum available allowing trainees to gain new insight into teaching [10].
Several radiology professional organizations recognize the need for assuring competence in as well as enthusiasm for the process of both peer and subordinate teaching in addition to confirmation of retention of learned material. The Radiologic Society of North America (RSNA) and the Association of University Radiologists (AUR) have in-person focused sessions and electronic support materials to develop and promote radiology educators.
Specific to radiology residency, there are few published reports of an integrated learning pathway to develop basic skills necessary to be effective in the role of educator, such as those described at the University of Pennsylvania and Emory University [11,12]. The program we have developed for imaging trainees, the Pathway for Added Certification in Education (PACE), provides a fully integrated experience to master these skills. This longitudinal curriculum provides education in a manner that is robust, but not competitive to the ongoing curriculum in Diagnostic Radiology (DR) or Nuclear Medicine (NM).
By design, this is a selective program, limiting the group size. We chose to limit the number of participants to assure attention to individual learning as well as commitment to the curriculum. In addition, limiting size allows for more tailored schedules for assignments and tasks that do not compete with training program requirements. We based the structure of the program on the tenets of technical presentation, personal presentation, and education principles.
Imaging lectures are typically supported by electronic media, providing text and especially figures. Power- Point was chosen as the predominant tool to develop given its wide use and likely familiarity to trainees. However, most pre-existing skills were self-taught and were bare bones techniques that could apply to any clinical setting. Our training provided imaging-specific tips and tricks. Further, general aesthetic enhancements were reviewed, aiming to increase learner focus as well as enjoyment. Although not essential, we also introduced another technical platform (usually Prezi) to increase the repertoire and stimulate creativity for presentations.
Despite a snazzy presentation, however, lectures may fall flat with poor personal presentation. We noted a common theme that our younger colleagues, as perpetual students, needed to be reminded about the importance of first impressions [13]. Particularly with limited time for instruction, this program stressed best practices for buying credibility for their knowledge and expertise. Participants had the opportunity to learn about physical appearance and universal body language.
The last element of the program focused on providing a review of literature and digital resources exploring the types of learners and learning environments. Program participants learned about expectations and limited time resources that may limit success in an adult learner environment [14]. A variety of resources were included such as printed literature and TED Talks (https://www. ted.com) to maximize viewpoints [14,15].
As our program advances into the 9th year, validation of the success of this long-running program was warranted. We utilized a Microsoft Forms anonymous electronic survey since the majority of the PACE program graduates are no longer affiliated with our institution. We used a peer-matched cohort from our training program for comparison. The survey developed was two- pronged, with one arm addressing background (such as pre-residency experience as educator), and one arm addressing PACE program elements. Drawing numerical conclusions is challenging given the low number of PACE participants for this cohort. However, some distinct trends were evident.
As a good starting point, only 1 of 24 respondents had received prior formal education for the role of teacher, giving most respondents a similar starting point. Overall, assessment of the value of the program by PACE participants was positive, with individual comments indicating that new information was provided, and skill set was advanced by participating in the program. Ranking of specific elements of the program revealed that the technical and personal presentation components were the most valued. Fortunately, no substantial interference with their duties as resident trainees was noted. These findings validate both the intent and the implementation of this program.
Surveys from both cohorts listed current commitments to providing education for medical students, residents, and/or peers. However, there was increased confidence in personal teaching skills reported for the PACE cohort (4.1/5 compared with 3.6/5). We acknowledge that responses submitted for elements such as perception of presentation success and confidence in personal skills are likely biased since based in introspection. However, overall presentation success is strongly linked with intangible elements such as confidence [16,17].
The results of this study validate the utility of our training program, although a few factors must be considered when interpreting results. The total number of PACE participants is small, precluding rigorous statistical analysis. However, every educational program should periodically evaluate the success of the endeavor, and a 10-year interval is satisfactory. Similarly, it would have added power to the analysis if all surveys had been completed, but this is an impractical expectation for an anonymous voluntary survey. Further, many of the survey questions are subjective, allowing bias. This bias is acceptable given that many of the elements of a successful public presentation are based on intangibles such as the confidence of the speaker.
This program was developed to support and inspire developing imaging colleagues in the combined science and art of medical education specific to imagers. Participation in medical education can occur in many different types of medical practice, but teaching is a frequent mandate in an academic institution. Therefore, the strong survey trend for PACE participants to join academic practice compared to non-PACE participants (6/6 PACE graduates, 3/11 non-PACE graduates) supports success in our goal to foster this outcome. This finding has a strong implication for the importance of supporting our future radiology educators early in their career. The premise can certainly be extrapolated to other medical subspecialities.
Conclusion
Providing training in the basic elements of scholastic presentation through an integrated, non-competitive training opportunity such as PACE, junior colleagues can develop and expand skills as well as confidence to create a successful learning environment. We are optimistic that such programs will have a positive effect in training future educators.
References
- Mukhalalati BA, Taylor A. Adult learning theories in context: A quick guide for healthcare professional educators. J Med Educ Curric Dev 2019;6:2382120519840332.
[Crossref] [Google Scholar] [Pubmed]
- Cheng WC, Lin XZ, Chen CY. Using modern teaching strategies to teach upper abdominal sonography to medical students. J Chin Med Assoc 2013;76(7):395-400.
[Crossref] [Google Scholar] [Pubmed]
- TED Talks: Discover ideas worth spreading.
- Create a presentation in PowerPoint for the web. Microsoft 2024.
- Allen BR. Transition to Practice: From Resident to Faculty at the Same Institution. J Grad Med Educ 2014;6(4):799-800.
[Crossref] [Google Scholar] [Pubmed]
- Kensinger CD, Mcmaster WG, Vella MA, Sexton KW, Snyder RA, Terhune KP. Residents as educators: A modern model. J Surg Educ 2015;72(5):949-956.
[Crossref] [Google Scholar] [Pubmed]
- Habboush Y, Stoner A, Torres C, Beidas S. Implementing a clinical-educator curriculum to enrich internal medicine residents’ teaching capacity. BMC Med Educ 2019;19:1-2.
[Crossref] [Google Scholar] [Pubmed]
- Goals, Learning Objectives, and Outcome Goals. Medical Education Track 2023.
[https://med.emory.edu/education/gme/housestaff/residency-tracks/medical-education.html]
- Three phase structure of the four years of the new curriculum. Downstate Health Science University.
[https://www.downstate.edu/education-training/college-of-medicine/curriculum/curriculum-map.html]
- Residents as Educators.2021.
[https://www.stfm.org/teachingresources/curriculum/residentsaseducatorscurriculum/overview/]
- Tomorrow’s Educators and Clinicians in Healthcare (TEACH). Penn Medicine 2023.
- Peterson RB, Tuburan S, Ho C, Awan O, Mendoza DP, Mullins ME. Conquering educational mountains: Maintaining a radiology clinical education track. J Am Coll Radiol 2023;20(3):364-368.
[Crossref] [Google Scholar] [Pubmed]
- Presentations: The poser of first impressions.
[https://franchetti.com/presentations-the-power-of-first-impressions]
- Lake FR. Teaching on the run tips: Doctors as teachers. Med J Aust 2004;180(8):415.
[Crossref] [Google Scholar] [Pubmed]
- Horii CV. Teaching insights from adult learning theory. J Vet Med Educ 2007;34(4):369-376.
[Crossref] [Google Scholar] [Pubmed]
- Farley J, Risko E. Everyday attention and lecture retention: The effects of time, fidgeting, and mind wandering. Front Psychol 2013;4:57742.
[Crossref] [Google Scholar] [Pubmed]
- Nadiah N. The students’ self-confidence in public speaking. Elite J 2019;1(1):1-2.
Appendix
1. What description best describes your current practice?
Academic with radiology residents/fellows; Academic or private practice with non-radiology trainees; Private practice with no trainees; Government/military; In residency/ fellowship; Other.
2. Of the following groups, to which learners do you provide focused training/lectures?
Select all that apply: Medical students; Radiology/Nuclear Medicine trainees; Non-Radiology trainees; Peer colleagues; Regional meetings; National meetings; International meetings; None.
3. About how many lectures do you provide per month?
0; 1 to 3; Greater than 3.
4. Which single group represents the largest percentage for your lectures?
Medical students; Radiology/Nuclear Medicine trainees; Non-Radiology trainees; Peer colleagues; Regional meetings; National meetings; International meetings; None.
5. Please rank your confidence levels for the following skills for public presentations/lectures?
0 is no confidence and 5 is very confident; Technical (computer software); Verbal; Body language; Overall confidence/skills.
6. During residency, do you feel there was sufficient opportunity to develop your presentation/public speaking skills (e.g. Grand Rounds, Journal Club, etc)?
Yes; No.
7. During your job/fellowship application process, was there any inquiry about your educational/teaching skills from potential employers?
Yes; No; Don’t remember
8. Did you participate in the PACE program?
Yes; No; Non-PACE trainee questions.
9A. Have you received any formal training in teaching adult learners?
Yes; No.
10A. Have you rec
Yes; No.
11A. Has anyone critiqued or coached you regarding presentation skills?
Yes; No.
12A. In retrospect, would you have participated in the PACE program to help develop presentation skills?
Yes; No.
13A. Do you think participation in the PACE program would have enhanced your job application?
Yes; No.
14A. Do you think participation in the PACE program would have helped you in your current job duties?
Yes; No; PACE participant questions.
9B. Prior to PACE, did you receive any formal training in teaching adult learners?
Yes; No.
10B. Prior to PACE, did you receive any formal training in technical computer skills e.g. developing PowerPoint presentations?
Yes; No.
11B. For how many years did you participate in the PACE program?
1; 2; 3; 4.
12B. What was your dominant reason for applying to PACE?
Interested in Topic; Identified need to enhance skill set; Enhanced CV; Coercion by mentors; Other
13B. What were your anticipated rewards before starting the program? Select all that apply?
Understanding the science of the education process; Improved presentation skills; Increased confidence with public speaking; Enhanced CV; Added benefit to academic job application; Getting to know the mentors; Other.
14B. How would you rate the workload required as a participant of this program for each component?
0 is no work and 5 is overwhelming workload; Serving as a medical student liaison; Learning technical computer programs; Techniques of oral presentation; Review of education articles/electronic presentations; Overall educational value.
15B. To what degree did the overall workload interfere with your radiology training?
0 is no interference and 5 is extreme interference.
16B. How would you rate the educational value of each component?.
0 is no educational value and 5 is high educational value; Serving as a medical student liaison; Learning technical computer programs; Techniques of oral pre sentation; Review of education articles/electronic presentations; Overall educational value.
17B. What was the highest yield component for you?
Serving as medical student liaison; Learning technical computer programs; Techniques of oral presentation; Review of education articles/electronic presentations; Other.
18B. How would you rate all your program mentors in the following categories?
0 is poor and 5 is excellent; Knowledge of material; Approachability; Individual interaction/engagement; Enthusiasm for task; Overall mentor rating.
19B. What was your impression of rewards at the conclusion of the program?
0 is no rewards and 5 is very rewarding.
20B. Did the PACE program influence your decision to pursue academic practice?
Yes; No; Unsure; I did not pursue academic practice.
21B. Did the PACE program influence your decision to act as a mentor for trainees in your job / fellowship?
Yes; No; Unsure; I did/do not act as a mentor for trainees.
22B. Did you think the PACE program was beneficial in acquiring a job/fellowship?
Yes; No; Unsure.
23B. During your job/fellowship application process, was there any inquiry/verbalized interest in the PACE program from potential employers?
Yes; No; Don’t remember.
24B. Have you had the opportunity to apply the concepts learned in the PACE program to your job/fellowship activities?
Yes; No.
25B. What has been the largest realized benefit of this program in retrospect?
Understanding the science of the education process; Improved presentation skills; Increased confidence with public speaking; Enhanced CV; Added benefit to academic job application; Getting to know mentors; None; Other.
26B. If you were redesigning the program, what element would you remove?
Serving as medical student liaison; Learning technical computer programs; Techniques of oral presentation; Review of education articles/electronic presentations; None of the above; Other.
27B. Please state any program positives not mentioned above.
28B. Please state any program negatives not mentioned above.